Immune rejuvenation could pave the way for healthier aging
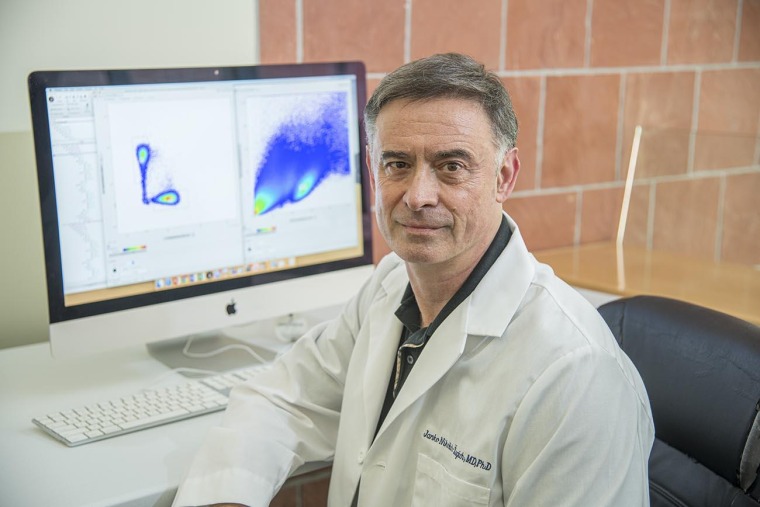
As we grow older, our immune systems weaken, making us more susceptible to infections and other diseases. As part of a long-running research program to develop strategies for “rejuvenating” the aging immune system, the National Institute on Aging has awarded a $13.1 million grant to a team of investigators across the country led by Janko Ž. Nikolich, MD, PhD, professor and head of the Department of Immunobiology at the University of Arizona College of Medicine – Tucson.
“This grant brings several projects together, reaching across the U.S. from Arizona to New York to Seattle to Texas and back,” Dr. Nikolich said, adding that each team is focusing on one piece of the larger puzzle. “To make sure we can actually improve the aging immune system, we’re researching immune rejuvenation from several angles.”
The Nikolich Lab initially focused their studies on T cells, which patrol the bloodstream to defend against bacteria, viruses and other pathogens. Their findings, however, led them to lymph nodes, which Dr. Nikolich describes as “outposts” scattered throughout the body where T cells prepare for battle. A portion of the current grant will support the Nikolich Lab’s investigations into how the lymph nodes deteriorate with age — and how they might be rejuvenated to help defend against disease even as we grow older.
Aging and immunity
A healthy child produces millions of new T cells daily to keep the supply fresh. These “naïve” T cells have never responded to an infection and are important in helping us respond to pathogens we haven’t previously encountered.

“The role of naïve T cells is to be ready for an attack by any microorganism,” Dr. Nikolich said. “The naïve cells are like the Department of Defense. There’s huge numbers of new soldiers, and you need the infantry, Air Force, engineers — all these guys around to protect you from danger. Many of them will never be deployed, but it is critically important that we have enough.”
Naïve T cells detect pathogens in the lymph nodes, where now-activated T cells begin to multiply and arm themselves for combat.
“That process takes several days,” Dr. Nikolich said. “Usually, somewhere around day four to seven, we start seeing these cells in the battlefield in larger numbers. They leave the lymph nodes armed with a lot of antimicrobial molecules, and then hunt down pathogens and kill them.”
Previous studies by the Nikolich Lab discovered that as we age, naïve T cell production drops, which impacts the immune system’s ability to recognize new pathogens. This aspect of the aging process kicks in much earlier than one would expect.
“Between puberty and early adulthood, the production of naïve T cells drops tenfold. There is another tenfold loss between the age of 40 and 50,” Dr. Nikolich said. “That would be OK if we could maintain what we have, but in the latest third of life, the lymph nodes start failing at maintaining the naïve T cells. We’re interested in both jumpstarting the production and improving the maintenance of naïve T cells.”
His team is collaborating with labs across the country to investigate strategies for kickstarting the aging immune system. The Nikolich Lab is investigating how to rejuvenate older immune systems to produce naïve T cells that respond to new infections just as robustly as T cells in younger immune systems.
Responding to surprises
In previous studies, the Nikolich Lab used a growth factor and a hormonal therapy to trigger T cell production in animal models, but the new cells didn’t circulate through the body to do their jobs.

“We can get new cells made. We saw them go into the bloodstream on the way to the lymph nodes, but they didn’t stay in the lymph nodes to prepare for battle,” he said. “That was surprising to us.”
These unexpected results forced the team to take a closer look. It turns out that the lymph nodes may be an important piece of the puzzle.
“We thought the aging T cells were the problem, but when we did some very careful experiments, it turned out that if you take rejuvenated T cells and put them in old lymph nodes, they don’t work well,” Dr. Nikolich said. “That’s telling us that we’ve been looking at this entirely wrong, and that we need to focus on what’s happening within the lymph nodes.”
Further investigation revealed that lymph nodes deteriorate with age.
“Even if you have enough T cells, if they don’t have outposts from which they can prepare for battle, they’re not going to be able to defend the organism,” Dr. Nikolich said. “Eventually, if we’re going to fix the whole system, we will have to fix the lymph nodes. How we can fix them is going to be the question for the next five years — or hopefully less.”
Looking toward the future
Dr. Nikolich hopes his group’s discoveries will open doors to a wide range of advances in improving immunity in older people, from vaccines that are more effective in aging immune systems to improved cancer treatments.
“One of the goals of aging research is to extend the function of different organs and systems in the body, so that whatever years we have to live, we can have a good quality of life,” he said.
Dr. Nikolich uses the example of the COVID-19 pandemic to illustrate why it’s so important to pay attention to immunity across all stages of life.
“Older adults are a lot more susceptible to infection, and cannot quite mount new responses as efficiently, as robustly, and as timely as they need,” he said. “As a consequence, we had these absolutely devastating statistics that, when infected with coronavirus before the advent of vaccines, people over the age of 80 were dying 270 times more than folks between 18 and 39. That tells you how much more susceptible older adults are.”
Dr. Nikolich’s interests in gerontology and immunity have driven his decades-long career, but the COVID-19 pandemic affected him in a deeply personal way.
“The pandemic has certainly reminded me and my colleagues why we went into this line of work. If I needed any additional motivation, I lost both parents to COVID,” he said. “Infectious diseases have always been the biggest killer on this planet until the 1960s or so, but the COVID-19 pandemic warns that infections remain dangerous and deadly. We still have a lot of work to do.”
This work is supported by the National Institute on Aging, a division of the National Institutes of Health, under award No. 2P01AG052359-06, and is part of a collaborative research effort that also includes investigators from the Fred Hutchinson Cancer Research Center, the Memorial Sloan Kettering Cancer Center, University of Texas at Austin, MD Anderson Cancer Center and Arizona State University.

