To accelerate search for an Alzheimer’s cure, scientists use artificial intelligence to identify likely drug targets
One of medicine’s most perplexing problems is Alzheimer’s disease, a neurodegenerative disorder that causes dementia, memory loss, personality changes and other irreversible symptoms. Drugs can treat symptoms of the disease, but a cure has been a challenge — possibly because the cause of Alzheimer’s disease is unclear.
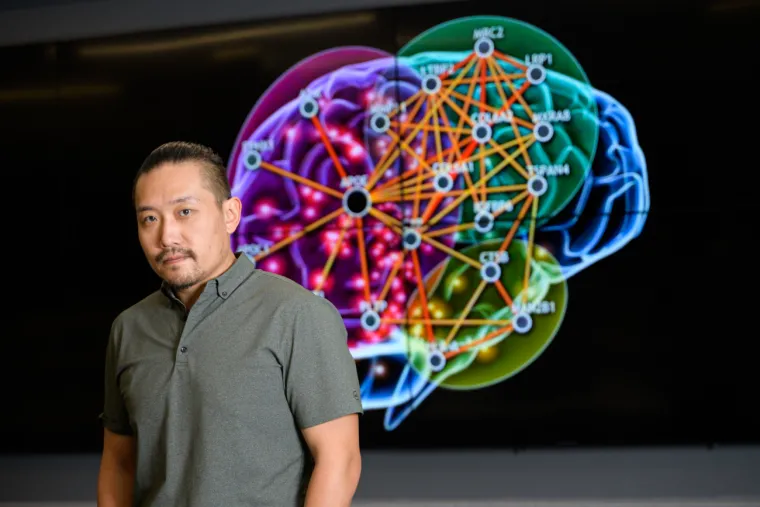
A team led by Rui Chang, PhD, associate professor of neurology at the University of Arizona College of Medicine – Tucson, along with collaborators at Harvard University, harnessed artificial intelligence to pinpoint Alzheimer’s causes, looking deep into the human brain to map the molecular changes that healthy neurons undergo as the disease progresses. The results were published today in Nature Communications Biology.
Mapping pathways to trace Alzheimer’s journey
“There are multiple pathways involved in Alzheimer’s disease,” Dr. Chang said, referring to the sequence of events that occur within cells to trigger changes in the body. For a long time, researchers focused on the buildup of telltale “amyloid plaques” and “tau tangles,” abnormal structures in the Alzheimer’s brain, as previous studies showed an association between these brain abnormalities and the disease. However, drugs clearing away and halting production of plaques and tangles have failed in clinical trials — pointing to the likelihood that they aren’t a cause of Alzheimer’s, but rather a consequence of earlier events.
Dr. Chang likens the path from health to Alzheimer’s to a watercourse in which the plaques and tangles occur “downstream” in response to problems occurring “upstream.”
“Amyloid plaques and tau tangles are downstream effects of a series of genetic mutations in upstream pathways that induce Alzheimer’s. It’s very doubtful that targeting these abnormal structures directly will be effective. In my perspective, the correct way is to target the disease upstream,” Dr. Chang said. “Therefore, it is critical to understand the whole landscape.”
Dr. Chang uses AI to map this landscape. With tissue samples from more than 2,000 Alzheimer’s brains taken from a national database, Dr. Chang’s AI algorithm drew from a deep well of information about genetic and molecular processes, returning a computational network model of the human brain. His team can now see maps of genes that work together across the whole genome, and can track the sequential changes in these genes’ relationships as Alzheimer’s develops, providing clues to the disease’s origins and tracing the molecular path from health to disease.
“The AI is a novel method that can tease apart massive data into a network model to provide a crystal-clear picture of upstream events, showing which upstream genes control important downstream genes,” Dr. Chang said. “With that model, we are able to pinpoint the upstream genes that trigger amyloid plaques and tau tangles downstream. These upstream genes may be better targets for potential therapies.”
Examining these genes individually in a traditional lab would be time consuming, so the scientists’ approach is to leverage high-powered computing and AI to select the most promising targets for precision medicine.
“This is not studying one gene by one gene — it’s 6,000 targets all at the same time, which will significantly accelerate drug development and discovery,” Dr. Chang said. “This is the first study showing that the AI and big data-driven approach could open the door to develop treatment for Alzheimer’s by targeting new pathways or combinations of pathways.”
Finding targets and the drugs that hit them
Dr. Chang used AI to help identify 19 particularly interesting neuron-specific genetic points on the Alzheimer’s pathway that appear to push neurons closer toward a disease state. Study collaborators at Harvard validated these genes’ role in Alzheimer’s development by using stem cells to create neurons in petri dishes and then deactivating the genes to see what would happen. They found that 10 of these genes affected production of plaques and tangles, and could be investigated as targets for drugs to treat Alzheimer’s.
“If deactivating these genes significantly changes the levels of amyloid plaques and tau tangles, then this is a validated target to develop treatments for Alzheimer’s disease,” Dr. Chang said.
Once gene targets are identified, the next step is to find drugs that will hit those targets. Once again, high-throughput computational power is leveraged in place of tedious and time-consuming laboratory experiments. 3D computer models determine if existing molecules and drugs might fit into potential drug targets like a lock into a key.
These experiments helped the team virtually screen millions of Food and Drug Administration-approved, natural product and small-molecule compounds against more than 6,000 targets, narrowing the field to about 3,000 drug candidates of interest. Along with several small molecules they are investigating further, the team already has a National Institutes of Health grant enabling clinical trials on three of the compounds. They expect human trials to start soon.
“Starting from mathematics and data, I can design mathematical algorithms to lift up a massive amount of data all the way to clinical studies in patients,” Dr. Chang said. “To see the compounds going into clinical trials and finally benefit patients is a fascinating journey for me.”
Leveraging computational power to solve health challenges
The AI was originally coded by Dr. Chang, and he has used it to conduct similar studies in conditions such as melanoma, diabetes and cardiovascular disease, making his team the first to use artificial intelligence to find genetic targets in a wide range of diseases. He is cautiously optimistic that AI can accelerate precision medicine research in many of medicine’s most vexing problems.

“We’re hopeful that AI is a game changer,” Dr. Chang said. “In five years, I hope there are more clinical trials for drugs for treatment of Alzheimer’s disease, and in 10 years, I hope there will be a couple of FDA-approved drugs to stop or potentially reverse disease progression.”
Dr. Chang’s doctorate is in computer science, specializing in AI and machine learning, and he has been applying his skills to genomic data for more than 15 years. He says the opportunity to work at the intersection of computation and biology has been enormously rewarding.
“The brain is a fascinating organ because it defines us as human beings,” he said. “There are a lot more complex functions not discovered yet that may unlock some hidden doors.”
This research was conducted using a database made available by the Accelerating Medicines Partnership® Program for Alzheimer’s Disease (AMP® AD), a public-private partnership between the National Institutes of Health (NIH), the U.S. Food and Drug Administration (FDA), multiple biopharmaceutical and life science companies, and nonprofit organizations, to transform the current model for developing new diagnostics and treatments for Alzheimer’s disease. This work was supported in part by the National Institute on Aging, a division of the National Institutes of Health, under award Nos. 1R56AG062620-01, 1RF1AG057457-01, R01AG055909 and RF1NS117446, the National Institute of Neurological Disorders and Stroke, a division of NIH, under award No. U54NS110435, and the UArizona Center for Innovation in Brain Science.

