A better way to study Parkinson’s disease in the lab could lead to earlier diagnosis
Detecting the neurodegenerative disease at an earlier stage might open doors to more effective and targeted treatments.
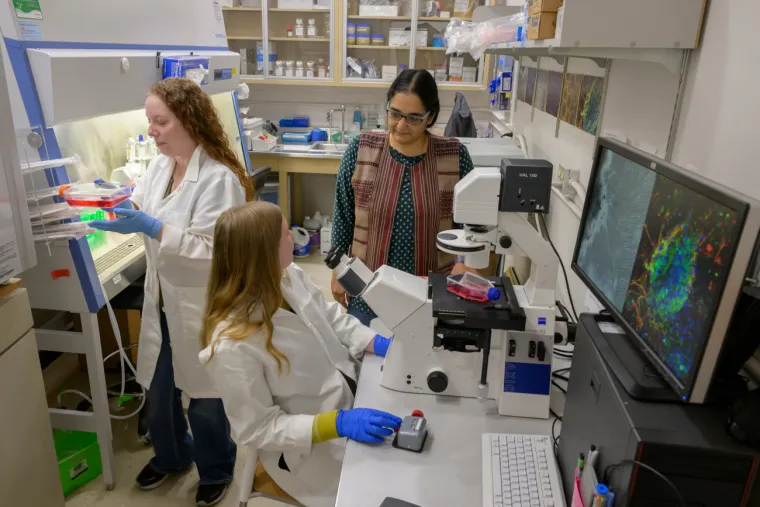
The Madhavan Lab hopes their discoveries will lead to improved diagnostics and treatments for Parkinson’s disease.
Kris Hanning
Around a million Americans are living with Parkinson’s disease, a neurological disorder that causes difficulty in movement, balance and cognition. Symptoms worsen until tasks like walking, talking and swallowing present enormous challenges. While there is no cure, there are treatments that control symptoms — but their effectiveness wanes over time and they are associated with unwanted side effects.
A recent study in Progress in Neurobiology, led by Lalitha Madhavan, MD, PhD, associate professor of neurology at the University of Arizona College of Medicine – Tucson, has developed an improved method to study Parkinson’s disease in the lab. Along the way, the lab has also uncovered clues that may help scientists figure out how to detect Parkinson’s earlier — and point the way toward better treatments.
“It’s a slow-developing disorder. We only diagnose the disease at a late stage, when 60% to 70% of dopamine neurons are dysfunctional or have died off,” Dr. Madhavan said. “We have treatments, but at that point you’re trying to throw a small glass of water on a raging fire. Being able to diagnose the condition at the earliest stages would be a big step.”
A better lab model
Dr. Madhavan says the original intention behind their work was to create a better tool with which to study Parkinson’s disease in the lab. Scientists have conducted the bulk of Parkinson’s laboratory research in animal models or animal cell cultures.
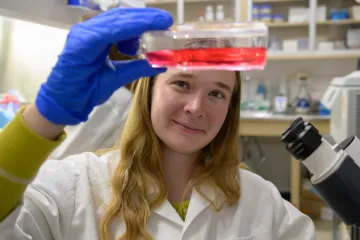
Aiden McRobbie-Johnson, graduate student in the Madhavan Lab, looks at a flask of skin cells.
Kris Hanning
“This has been what the field has been working with for many years, and it’s provided important insights into the disease — but it doesn’t capture the human system,” she said.
As an alternative, Dr. Madhavan’s team used cells from Parkinson’s patients to create a human-derived system. Using induced pluripotent stem cell (iPSC) technology — a powerful technique that transforms adult cells into embryo-like cells that can then mature into any cell type — the lab reprogrammed adult skin cells called fibroblasts into brain cells.
“Genetic reprogramming technologies have changed the field tremendously,” Dr. Madhavan said. “We can isolate skin cells from living individuals with Parkinson’s and drive them to become neurons.”
Using the reprogrammed neurons, the Madhavan Lab discovered several changes in the cells from Parkinson’s subjects that differentiated them from cells of healthy individuals. Dr. Madhavan hopes this finding can form the basis for better cell-culture systems for studying Parkinson’s disease in the lab, potentially leading to improved diagnostics and treatments.
Catching Parkinson’s earlier
These experiments also showed that skin cells may act as a window into the brain. Although skin cells don’t cause neurological symptoms, some of the same changes that damage brain cells might also affect skin cells, producing similar molecular “signatures.” The team hopes that, in the future, doctors will be able to catch Parkinson’s disease earlier by examining skin cells for signs that the disease is brewing.

Dr. Lalitha Madhavan (right) oversees a lab whose discoveries in skin cells could help scientists take a closer look at brain cells.
Kris Hanning
“This could be a system in which we could very carefully diagnose people at early stages,” Dr. Madhavan said, adding that her team received a patent on a method for examining skin cells for molecular signs that correlate to Parkinson’s disease. They are now investigating how skin cells change over time to learn more about how the disease progresses and how to identify it early. Tech Launch Arizona, the University of Arizona’s technology commercialization office, is helping the team through the process of protecting the innovation and developing strategies to take it from the laboratory to the marketplace where it can impact the lives patients and their doctors.
Dr. Madhavan says that, if we could catch Parkinson’s disease earlier, doctors could prescribe currently available treatments that can slow disease progression. Simultaneously, scientists could work to develop next-generation Parkinson’s drugs that target the disease in its early stages.
Because a patient’s skin cells are easy to access — especially compared to brain cells — Dr. Madhavan also hopes the system could be used for a precision-medicine approach, matching patients with optimized treatments based on a skin biopsy and lab test showing which drug might work best based on their unique genetic profile.
“We’ve been putting Parkinson’s into one big bucket when actually different people express it differently,” she said. “This system would allow us to carefully classify Parkinson’s and assess treatments more effectively based on such a classification.”
An unexpected twist
While the team accomplished their goal of creating a human-derived system for studying Parkinson’s disease, they didn’t expect to stumble upon a potential strategy for early diagnosis. They were surprised to discover that the Parkinson’s signatures in the reprogrammed brain cells had been present in the original skin cells.
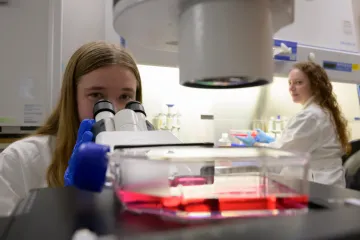
Dr. Lalitha Madhavan says students power the lab.
Kris Hanning
“We wanted to make neurons from skin biopsies using this fantastic technology. However, we noted along the way that the fibroblasts themselves seemed to have signatures that differentiated individuals with Parkinson’s. We started to dig deeper into that,” Dr. Madhavan said. “It’s exciting that we’ve shown that connection, and that it tells us skin cells could perhaps be used to diagnose the disease early.”
Dr. Madhavan says the road to discovery is filled with twists, turns and detours. Stumbling upon a potential technique for early diagnosis of Parkinson’s disease is one example of a happy surprise in the scientific journey.
“There’s a lot of serendipity in scientific research,” said Dr. Madhavan, who is also a member of the BIO5 Institute. “When doing science, going off on tangents is also important. The experiment is always telling you a story. We want to get to the truth, and nature is complicated.”
The study was supported mainly by a Michael J Fox Foundation Grant (MJFF 18366) to Dr. Madhavan, and grants from the National Eye Institute, a division of the National Institutes of Health, under award Nos. R01-EY-026027 and NSF-1552184 to EE. The lead authors on the study were Mandi Corenblum, MS, senior research specialist, and Aiden McRobbie-Johnson, physiological sciences graduate student. Co-authors include Kelsey Bernard and Timothy Maley, graduate students in neuroscience and physiological sciences; Emma Carruth, undergraduate student in physiology; Moulun Luo, PhD, associate research professor of medicine; Lawrence Mandarino, PhD, professor of medicine; Maria Sans-Fuentes, PhD, BIO5 Institute statistician; Dean Billheimer, PhD, director of statistical consulting at the BIO5 Institute; and Erika Eggers, PhD, professor of physiology and member of the BIO5 Institute.

