New Smart Bandage Blends Flexible Electronics and Wound Healing Science
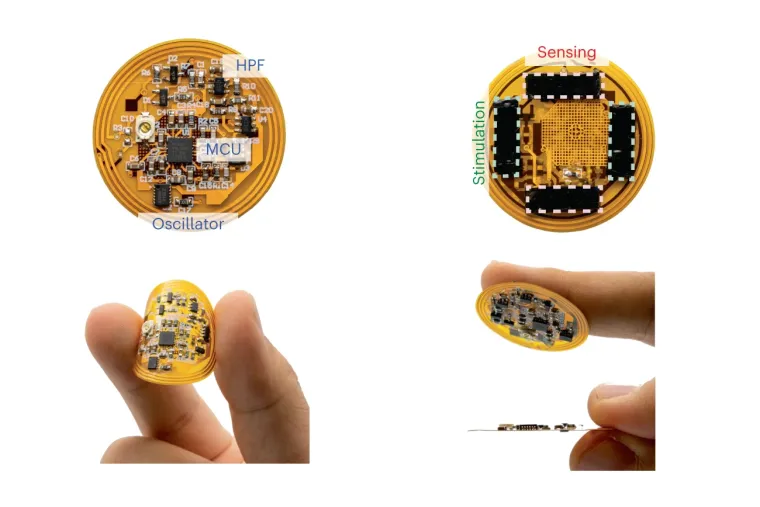
Image adapted from Nature Biotechnology (Nat Biotechnol) ISSN 1546-1696 (online) ISSN 1087-0156 (print)
Healing is a biological process that's easily taken for granted; you get a blister, scrape a knee or burn a finger, and after cleaning and bandaging the wound, the body takes over and starts the healing process. For some, however, the wound healing cycle becomes disrupted, impairing the body's ability to recover from even a simple cut.
The resulting chronic wounds can have a huge impact on a person's quality of life. They can cause severe pain, reduced mobility, emotional and physical distress, and isolation. In the most extreme cases, chronic wounds and resulting complications can even be fatal.
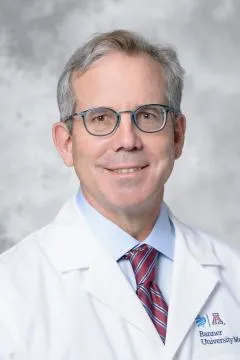
Finding effective treatments for chronic wounds has posed a significant challenge for scientists and clinicians. However, a new smart bandage developed by the labs of Geoffrey Gurtner, MD, FACS, chair of the Department of Surgery at the University of Arizona College of Medicine – Tucson, and Zhenan Bao, PhD, the K.K. Lee Professor in Chemical Engineering in the Stanford School of Engineering, presents a potential novel solution for improving chronic wound healing.
The bandage was introduced in a new paper published in Nature Biotechnology in November. It uses electrical stimulation and biosensors to help facilitate increased blood flow to the injured tissue, close wounds more quickly and reduce scar formation.
"This bandage would not only help wounds heal faster, especially for those struggling with chronic wounds, but the wireless sensors implanted in the bandage will also help physicians track in real time how a wound is doing," said co-first author Artem Trotsyuk, PhD, research assistant professor in the Department of Surgery.

The collaboration between the two biomedical engineering labs started at Stanford University back in 2018 through a shared interest in exploring how flexible electronics could be used in a clinical setting. The Bao Group had expertise in flexible electronics and chemical and electrical engineering. The Gurtner Lab, which moved to the UArizona College of Medicine – Tucson from Stanford this year, specialized in wound healing biology and patient care.
Together, the convergence of engineering, chemistry and medicine enabled the researchers to pair the well-studied possibilities of electrical stimulation with real-time biosensors, opening the door to what could be the next generation of technology to help patients with chronic wounds, Dr. Trotsyuk said.
"The future of patient care is interdisciplinary research," Dr. Gurtner said. "The Bao Group has been an invaluable partner, and we look forward to bringing the resources of the University of Arizona and Stanford University together to advance this research even further."
Dr. Trotsyuk and fellow co-first author Yuanwen Jiang, PhD, a post-doctoral scholar in the Bao Group, led their respective teams and worked together to build the device and design its subsequent studies.
"I led a lot of the clinical and biology exploration, and Dr. Jiang led a lot of the flexible electronics and hydrogel development," Dr. Trotsyuk said. "There were a lot of unknowns, but we built it out as time progressed — adding the right sensors, picking the right flexible board, et cetera."
The resulting technology includes a thin electrical layer that contains various sensors, wireless circuitry and an electronic stimulator. Underneath is a layer of hydrogel, a skin-like substance that adheres to the wound. Together, they measure the wound's healing progress and adjust the bandage's stimulation accordingly; if the wound is infected or healing too slowly, electrical stimulation will increase, in turn accelerating tissue closure.
Beyond designing and testing the technology, the team also wanted to understand how specifically electrical stimulation promotes wound healing. By running electrical current through the wound bed, they discovered that stimulation activates pro-regenerative and anti-inflammatory genes, while simultaneously recruiting more pro-regenerative white blood cells.
"Wound care biology is a field that provides the opportunity to develop therapeutics to help patients in very tangible ways," Dr. Trotsyuk said. "Being a part of this work that is so close to the bedside is incredibly rewarding."
Moving forward, the Gurtner Lab and the Bao Group will work to scale this technology up for application in humans. They still need to navigate challenges like data storage limitations and hydrogel rejection, but with the combined knowledge and creativity of two teams, Dr. Gurtner is confident one day these bandages will be used in clinics.
"I am excited about continuing this work at the University of Arizona and finding new ways to collaborate, expand on and strengthen this research to bring it to clinical translation," Dr. Gurtner said.
Contacts
Olivia Miltner

