Anesthesiology
About Our Residency Program
Welcome to the Anethesiology Residency Program at the University of Arizona College of Medicine – Tucson! Our residency program provides excellent clinical training, didactic education and subspecialty experience in a collegial environment. Each year, we welcome around 40 residents, ensuring individualized attention and a strong track record of success in academics and private practice.
As a medium-sized program without many subspecialty fellows, our program provides its residents the full spectrum of patient care while on their non-operating room rotations.
Advanced Anesthesia Services in Tucson: Collaborative Excellence
In partnership with Banner – University Medical Center Tucson, the University of Arizona Cancer Center, College of Nursing, College of Pharmacy, and leading research facilities, we foster a dynamic, collaborative environment. Our team expertly manages the operating suite and co-directs the surgical intensive care unit, providing top-tier surgical services to patients across Southern Arizona.
Comprehensive Training for Anesthesia Residents
Our residency program offers hands-on experience in a wide range of anesthesia subspecialties, from cardiovascular to trauma surgery. This ensures our residents meet the American Board of Anesthesiology’s case distribution requirements while gaining practical skills in real-world settings.
Specialized Surgical Expertise
We play a key role in advanced procedures, including:
- Cardiovascular and trauma surgery
- Organ transplantation (heart, kidney, lung, pancreas)
- Outpatient anesthesia services
Each year, our team administers over 15,000 anesthetics in 22 cutting-edge operating rooms and two dedicated obstetrical suites at Banner – University Medical Center Tucson. Our state-of-the-art facilities support exceptional patient care and surgical outcomes.
Integrated Care at Tucson Veterans Administration Medical Center (VAMC)
As part of our comprehensive program, we collaborate with the Tucson VAMC, a 240-bed facility serving veterans. Here, we deliver approximately 3,500 anesthetics annually, specializing in complex cases such as vascular, cardiac, neurological, and urological surgeries. Our work supports a diverse patient population with unique, co-existing conditions, ensuring high-quality care tailored to their needs.
To apply, submit the following materials by October 1 through ERAS and Central App:
- ERAS Common Application Form (CAF)
- Central App
- Curriculum Vitae
- Personal Statement
- Dean’s Letter
- USMLE or COMLEX Score Reports
- Minimum of three Letters of Recommendation
- Certified Copy of Medical School Transcript
For any questions about the application, please contact HELP@accessgme.com
We look forward to reviewing your application.
The Department of Anesthesiology performs clinical care, teaching and research at five facilities:
- The Banner – University Medical Center Tucson Campus: a 480-bed tertiary care hospital, Level-1 Trauma Center, and Regional Transplant Center for Southern Arizona; the primary teaching hospital for the College of Medicine – Tucson
- The Banner University Medical Center – South Campus
- Southern Arizona Veterans Administration Health Care System (SAVAHCS): a 285-bed hospital provides training, primary care and subspecialty health care in numerous medical areas
- The Banner University Medical Center – La Cholla Physician Offices – Northwest Office
Curriculum
Our residency program offers both a categorical track, which includes the first year of training (PGY-1), and an advanced three-year anesthesiology program that begins in the CA-1 year (PGY-2). In the categorical track, residents complete their first year as part of a full, four-year anesthesiology residency, while the advanced program allows residents to begin directly at the CA-1 (PGY-2) level after completing a preliminary year elsewhere.
Ambulatory Rotation
Residents are introduced to upper and lower extremity regional anesthesia early in their training. This rotation’s curriculum emphasizes the perioperative evaluation, preparation and management of patients undergoing same-day surgery.
Cardiothoracic Anesthesia
Anesthesia residents complete a four-month rotation in the intensive care unit (ICU), working in the Surgical Trauma ICU (STICU), a 20-bed unit alongside surgical intensivists, critical care fellows and emergency medicine residents. This rotation enhances their procedural skills, post-operative resuscitation and triage abilities. Residents also rotate through the cardiovascular ICU (CVICU), which cares for patients after complex cardiac procedures. Here, anesthesia residents take the lead in patient care under the guidance of anesthesia-trained intensivists.
Chronic Pain
Residents have the opportunity to partake in procedures that include but are not limited to: neuraxial based injections, trigger point injections, radiofrequency ablation and spinal cord stimulators. Residents interested in chronic pain for fellowship work side by side with chronic pain fellows and chronic pain attendings.
Critical Care Medicine
During their Surgical Trauma ICU rotation, residents enhance their procedural skills, post-operative resuscitation and triage abilities. ICU experience is further enriched by a rotation in the cardiovascular ICU (CVICU), which cares for patients after complex cardiac procedures, including revascularizations, valve replacements and ventricular assist device placements.
Neuroanesthesia
As a senior elective, residents can rotate at Barrows Neurological Institute in Phoenix, where they gain proficiency in the perioperative management of complex neurosurgical patients. They participate in various procedures, including craniotomies, aneurysm coilings and clippings, tumor resections, CSF shunting and major spine surgeries. This diverse case mix ensures residents exceed index case minimums before graduation.
Obstetric Anesthesia
During this rotation, residents gain proficiency in labor epidurals, combined spinal-epidurals and spinals for cesarean sections. The curriculum emphasizes the physiological changes that occur in parturient patients and how these affect anesthesia management. Residents complete three four-week rotations in obstetric anesthesia, providing a comprehensive experience that helps them easily meet case-log minimums.
Pediatric Anesthesia
Residents provide anesthetics for pediatric patients during their non-operating room anesthesia rotation in radiation oncology, MRI, CT and GI endoscopy. They encounter a diverse case mix, including complex neonatal cardiac surgeries and specialized pediatric procedures in neurosurgery, ophthalmology and otolaryngology. Without pediatric fellows in the program, residents work closely with a pediatric anesthesiologist during these intensive surgeries.
Pre-Anesthesia Clinic
Under faculty guidance, residents staff the pre-anesthesia clinic, where they assess patients referred for elective or urgent surgery. They familiarize themselves with the latest perioperative guidelines, counsel patients and develop pre-anesthetic plans prior to surgery.
Post Anesthesia Care Unit (PACU)
Early in training, residents work in the PACU, monitoring patients in immediate postoperative recovery. During this two-week rotation, they handle hypotension, airway emergencies, resuscitation and pain management with faculty guidance. By the end, residents develop the skills to independently evaluate and manage various postoperative complications.
Regional Anesthesia
Residents gain exposure to regional anesthesia in various clinical settings. On the Acute Pain Service at Banner – University Medical Center, they join a dedicated regional team as perioperative consultants, quickly mastering peripheral and neuraxial blocks for thoracic, abdominal, orthopedic, breast and vascular cases. This experience is enhanced by rotations at the Southern Arizona VA Health Care System and Banner – University Medical Center South Campus, where residents perform approximately 2,500 regional blockades annually. Senior residents can further rotate on the Acute Pain Service, taking on roles similar to a regional pain fellow.
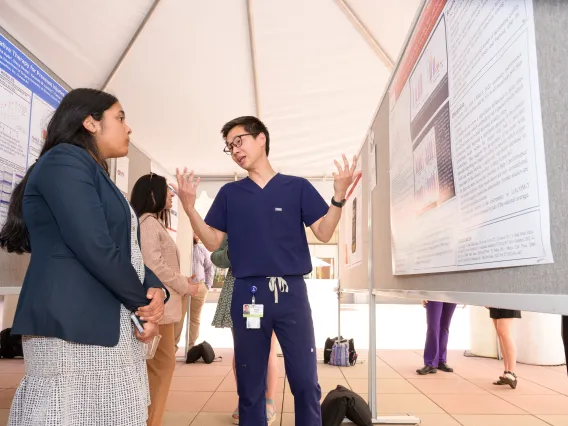
Research
Residents interested in research can engage in existing projects on topics like thromboelastography, snake venom’s anticoagulant effects, anesthesia and consciousness, the antinociceptive impact of green light and pediatric regional anesthesia adjuncts. They are also encouraged to pursue their own research questions with faculty support. Each year, residents present their work at various conferences, including the Western Anesthesia Regional Conference and the American Society of Anesthesiology’s annual conference, with reimbursement up to $1,000 for presentations.
Didactic Conferences
The Department of Anesthesiology conducts a three-year lecture series that aligns with the American Board of Anesthesiology content outline. These conferences use active learning methods, including Problem-Based Learning Discussions, interactive lectures and skills labs. Residents are expected to attend once a week.
In July, the didactic schedule adapts to support new residents with introductory lectures on topics such as airway management and anesthesia maintenance. This series helps them manage the extensive information required in anesthesiology.
Intraoperative Learning
Hands-on training occurs in the operating room, where faculty engage residents in discussions about cases and topics the night before.
Online Learning
CA-1 residents access Learnly, a structured online curriculum covering anesthesia basic sciences. They also use the Anesthesia Toolbox, which includes e-learning modules, quizzes, podcasts and procedural skills training guides. Discounts for a commonly used Qbank are provided to support success in exams.
Textbooks
CA-1s receive a personal iPad mini and anesthesiology textbook, including Morgan & Mikhail’s Clinical Anesthesiology and Barash’s Clinical Anesthesia.
Grand Rounds
Held weekly, Grand Rounds feature Continuous Quality Improvement Conferences, guest speakers, lectures and simulation sessions.
Journal Club
Residents present journal articles quarterly, covering various anesthesiology topics over dinner at a local restaurant.
Additional Resources
A range of supplementary learning resources is available, introduced during orientation, encouraging residents to explore what best supports their success.
Training in Tucson
Trish Angiulo
Residency Program Manager
vangiulo@arizona.edu
520-626-7141