Arizona Emergency Medicine Research Center
The Arizona Emergency Medicine Research Center is a collaborative statewide Center of Excellence dedicated to improving the health care outcomes of patients with acute illness and injuries, in both pre-hospital settings and within the hospital. Our research focus extends from the pre-hospital environment, including 911 and emergency medical services, through the emergency department and critical care settings.
About AEMRC
The mission of the Department of Emergency Medicine and Arizona Emergency Medicine Research Center is to improve lives through access to dedicated, high-quality clinical care, and cutting-edge scholarship, leadership and education. Our research strives for excellence to the extent that our peers consider our programs as a benchmark for scholarship. We are dedicated to fulfilling the land-grant institutional promises of caring for the diverse population of Arizona and greater Southwest. The tripartite partnership of our health care delivery network partner, Banner Health, the department and the center serves as an incubator for research, quality improvement and process initiatives with wide-ranging impact on the lives of those living in the Southwest and beyond.
The center brings together collaborative teams of multidisciplinary experts to achieve critical impact in areas affecting lives in Arizona today, including:
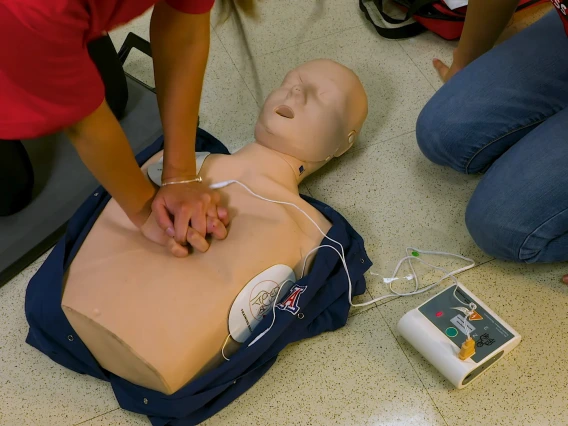
- improving outcomes in prehospital cardiac arrest
- prehospital traumatic brain injury
- emergency preparedness
- prehospital systems
- pediatrics
- clinical-translational medicine
- sepsis
- shock
- acute respiratory failure
- acute respiratory distress syndrome (ARDS)
- cardiac arrest
Department of Emergency Medicine faculty and the center regularly contribute research presentations at top scientific meetings in the United States and internationally. In addition, Department of Emergency Medicine residents participate in mentored research leading to national presentations and the publications.
The center has established a statewide clinical research network that conducts numerous studies, including clinical trials investigating neurological emergencies and cardiac arrest. The center has formed research collaborations with many University of Arizona colleges and departments, as well as with other universities in Arizona, the Southwest and internationally. Additionally, AEMRC has developed innovative collaborations with major and rural hospitals in Arizona serving diverse populations.
Arizona Emergency Medicine Research Center Tucson
AEMRC Tucson has a very active and growing research portfolio, including collaborations that bridge multiple departments and colleges across the state and the country. Research funding is diverse: private foundation, federal government, private businesses and state government, among others.
The strong focus and commitment to research is clearly demonstrated by the ScholarQuest project that leads each and every resident in the Department of Emergency Medicine through an original research project and its presentation. The AEMRC also supports an undergraduate and graduate program, the Research Associate Program, that encourages students to learn best practices in research and to participate in ongoing research projects.
AEMRC Tucson Leadership
Arizona Emergency Medicine Research Center Phoenix
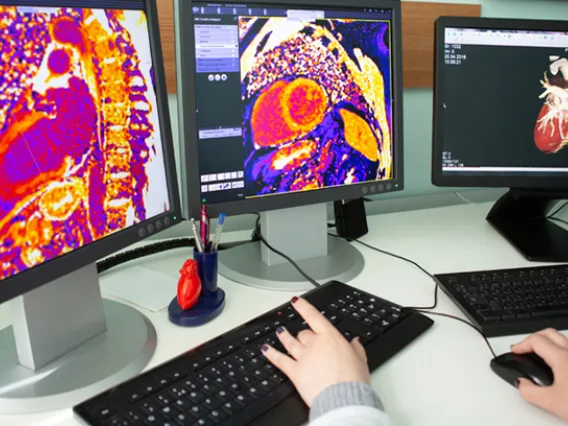
The Arizona Emergency Medicine Research Center (AEMRC) Phoenix is an internationally acclaimed hub for research focusing on improving outcomes for patients of time-sensitive cardiovascular, neurologic and traumatic medical emergencies. The AEMRC brings together a strong team of seasoned, NIH-funded, prehospital researchers concentrating on measuring and improving the effectiveness of life-saving prehospital medical interventions. The team includes expertise in epidemiology, database integration, advanced biostatistics and prehospital outcomes research.
AEMRC Phoenix Leadership
Advanced Hazmat Life Support (AHLS)

AHLS is a continuing education program of the Arizona Emergency Medicine Research Center.

The flagship 16-hour course sets the global standard for training health care professionals to care for people exposed to hazardous materials.

AHLS trains the trainers in a four-hour course followed with observation by an accomplished AHLS instructor, ensuring high teaching standards.

Additional continuing education courses cover radiological incidents and terrorism, toxic terrorism, chemical burns and toxic products of combustion, tox medics and tactical medics, and a basic hazmat life support online program.
Consumer Product Safety Commission

For more than 40 years, we have contracted with the Consumer Product Safety Commission (CPSC) to save lives and keep families safe by reducing unreasonable risk of injuries and death associated with consumer products. Medical records from the emergency department at Banner – University Medical Center Tucson are analyzed against National Electronic Injury Surveillance System database criteria, and pertinent encrypted data are submitted to CPSC.
University of Arizona Research Resources
Additional Research Resources
Funding Opportunities
Research Training & Education
CITI Protecting Human Research Subjects certification is valid for four years before refresher training must be completed.
This graduate certificate prepares clinician-scientists for the complexities of clinical research through high-quality didactic instruction and mentored research experiences.