NIH grant will help researchers follow a virus on its path to the nucleus
A University of Arizona College of Medicine – Tucson virologist’s work on human papillomavirus has been recognized by the National Institutes of Health for its enormous potential.
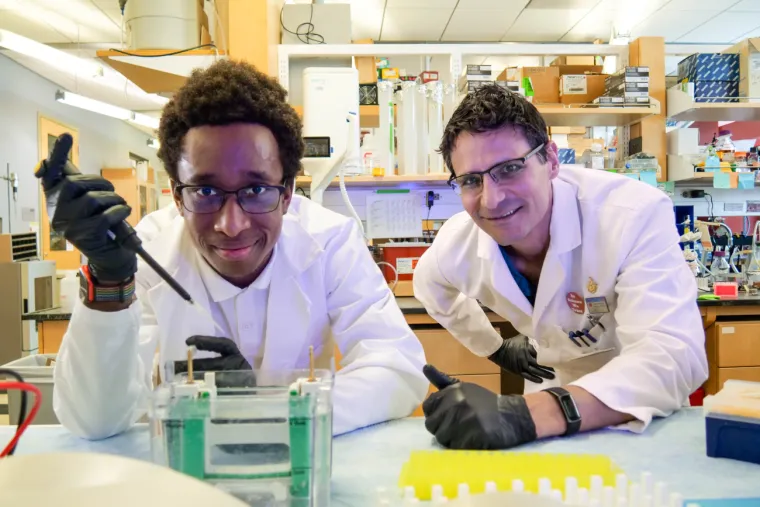
Chaz DeCoteau (left), an undergraduate double-majoring in biochemistry and pharmaceutical sciences, untangles the mysteries of human papillomavirus under the mentorship of Samuel Campos, PhD (right), associate professor of immunobiology.
Deanna R. Sanchez, BIO5 Institute
Human papillomavirus (HPV) can cause warts and certain cancers, and has been with us since the dawn of humanity. This tightknit relationship makes HPV an important source of information about our own biology, according to Samuel K. Campos, PhD, associate professor of immunobiology at the University of Arizona College of Medicine – Tucson and member of the BIO5 Institute.

Samuel Campos, PhD
Deanna R. Sanchez, BIO5 Institute
“These viruses take advantage of pathways the cell has and tweak them. What better cell biologists to teach us how cells work than the viruses that have evolved with us for eons?” Dr. Campos said about how HPV illuminates the innerworkings of our bodies. “Follow the biology of the virus, and we’ll learn some cool new cell biology.”
To delve deeper into their research on HPV, the Campos Lab was awarded a five-year $1.8 million R35 grant from the National Institutes of Health. This type of grant provides long-term funding that gives investigators flexibility to follow their research in whatever direction it takes them, and is reserved for scientists with outstanding research records and potential to make major contributions to their fields.
‘Constantly shedding’
Dr. Campos says there are more than 600 known strains of human papillomavirus, with more yet to be discovered. His lab mainly focuses on HPV16, the type that causes the majority of cervical, anal and head-and-neck cancers.
“Most HPV infections are cleared by the immune system, but there are so many infections out there that even the tiny fraction that aren’t cleared in a timely manner cause about 5% of cancers worldwide,” Dr. Campos said.
HPV has found its niche in certain types of epithelial cells, which cover our body as skin and line our body cavities as mucous membranes. The virus moves from the lower layers of the epithelium to the upper layers, and once it’s close to the surface, replication kicks into high gear as it prepares to leave one body and infect another.
“We are constantly shedding dead skin — it just comes off our body,” Dr. Campos said. “That is how they’ve so successfully spread throughout the human population.”
‘A wolf in sheep’s clothing’
HPV’s genes are packaged in a protein shell. The Campos Lab focuses on the role of one of these shell proteins, called L2, which can insert itself into the membranes of our cells, like a key into a lock, and let itself inside. Upon entry, the virus is escorted along a twisted path to the nucleus, where it hijacks the cell to make copies of itself.

Isabelle Tobey (left), a doctoral student in cancer biology, helps to move the Campos Lab’s research forward.
Deanna R. Sanchez, BIO5 Institute
Dr. Campos says his lab’s prior research revealed that, from the cell’s point of view, L2 looks like another part of the cell.
“We learned that the virus is really sneaky,” Dr. Campos said. “L2 can actually stick through the cell membrane without rupturing it, and HPV stays hidden behind these membranes. It’s able to avoid sensors that detect danger signals, like a wolf in sheep’s clothing.”
Previous research published by the Campos Lab and other groups suggested that HPV may be able to hide out until the cell’s machinery whirs into action during cell division, at which point it sheds its “sheep’s clothing” and hitches a ride to the nucleus.
“Once the virus has successfully delivered its DNA genome into the nucleus, it can begin expressing its own genes to take over the cell,” Dr. Campos said. “That will lead to immune evasion, alteration of the cell cycle, the generation of new viral particles, and transmission to another host. If the virus sticks around long enough, these infections can sometimes alter the cell in a way that leads to cancer.”
The grant will support the Campos Lab as they uncover how HPV takes advantage of cell division to move from its hiding place in the cell to the nucleus.
“It’s a complete black box. It’d be really neat to figure that out,” Dr. Campos said, adding that following the virus’s path will shed light on the intricacies of cell division and how things move in and out of cells.
‘A potent inhibitor’
The Campos Lab will use SNX-1.3, a type of small molecule known as a peptide, to explore how HPV initiates infection. Their previous work found that the peptide interferes with the virus’s ability to enter the cell.
“The peptide turned out to be a really potent inhibitor of HPV — it actually blocked the ability of L2 to stick through cell membranes in the first place,” he said. “We don’t understand how.”
Their hypothesis is that the peptide makes cell membranes less bendy and flexible, preventing L2 from creating weak spots through which to enter the cell. The grant will help them test this idea, which Dr. Campos hopes will uncover details of our own biology, though he doesn’t see potential in developing the peptide into a therapeutic to prevent HPV because there is already an excellent vaccine to block infection.
The lab’s use of SNX-1.3 arose from a chance encounter with Joyce Schroeder, PhD, professor of molecular and cellular biology and member of the UArizona Cancer Center. As she gave a presentation on this peptide, which her lab discovered while researching breast cancer, Dr. Campos’ ears perked up when she mentioned that it blocked the same pathway HPV uses to reach the nucleus.
“I was like, ‘Joyce, can I have some of your peptide to see if it would inhibit HPV?’ She was happy to give me her peptide to try,” he recalled. “That’s how most basic scientists are. We’re interested in getting answers to basic questions, and we’re usually happy to help each other out.”
‘Scratching my head about basic biology’
As a graduate student at Rice University, Dr. Campos conducted translational research aimed at creating new clinical procedures and therapeutics. But his work using viruses in gene therapy made him more interested in basic science — the foundational knowledge upon which translational science is built.

Under the mentorship of Samuel Campos, PhD (right), molecular and cellular biology doctoral students Ashlin Schaefbauer (left) and Zach Williamson (center) hope to learn how HPV travels to the center of the cell.
Deanna R. Sanchez, BIO5 Institute
“That gene therapy work was cool, but it got me scratching my head about the basic biology of how these viruses work,” he said. “There are so many facets of our own cell biology that have been illuminated by viruses.”
Dr. Campos says discoveries in basic science may not immediately lead to vaccines or cures, but those discoveries can lead other researchers down investigative pathways that may ultimately benefit patients.
For example, discoveries about HPV’s protein shell helped scientists develop the HPV vaccine, which primes the immune system to recognize another viral protein, L1, and neutralize the virus before it can infect a cell.
“We’re just trying to understand the basics of how cells work, how viruses work, and how they interplay together,” Dr. Campos said. “Who knows where this stuff will lead? Maybe it would lead to a great Ebola antiviral, who knows?”
These unknowns are what keep Dr. Campos coming to work each day.
“It’s tough and it’s frustrating, but it’s also satisfying — like solving a puzzle,” he said. “You don’t know where the science will take you. You don’t know what the ending is going to be. That’s exciting.”
This research is supported by the National Institute of General Medical Sciences, a division of the National Institutes of Health, under award No. 1R35GM152143-01.

