Department of Medicine
Nephrology
We strive to ensure an outstanding educational environment through exposure to a wide breadth of kidney diseases in a variety of clinical settings taking a fellow-centric approach. Our faculty are invested in shaping the next generation of nephrologists and promoting a supportive teaching environment tailored to the individual fellow. Our program has the right complement of trainees and rotations to ensure a positive work-life balance. Upon completion, our graduates demonstrate outstanding skill in all aspects of care in patients with kidney disease and are well prepared for a career in clinical practice or academic nephrology. Most important, our fellows develop a true passion for this wonderful subspecialty.
We look forward to making your training an exciting and educational experience!
Nephrology Fellowship Program
Our two-year clinical program is accredited by the ACGME/RRC and offers exceptional training in nephrology, with an optional third year available for those interested in clinical/translational research or intervention. We accept three fellows per year into this highly regarded program, which has been shaping skilled nephrologists since 1976.
Exceptional Training Opportunities
Outstanding Critical Care Training
- Level I trauma and tertiary care referral center
- Regional hub for ECMO (extracorporeal membrane oxygenation)
- Expertise in cardiac assist devices, including the total artificial heart
Comprehensive Transplant Experience
- Over 120 kidney transplants annually, including simultaneous pancreas-kidney transplants
- Heart, lung and liver transplantation
- Blood and marrow transplantation
Specialized Skills Development
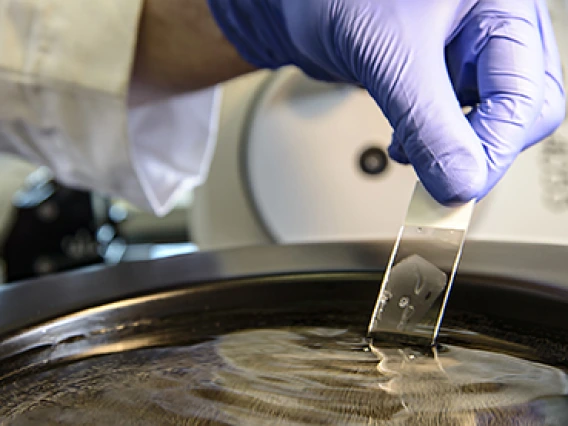
- Apheresis training
- Interventional nephrology
- Strong focus on home dialysis therapies
- Urgent-start peritoneal dialysis program
Advanced Clinical Exposure
- Robust experience with glomerulonephritis patients
Personalized Career Support
We provide individualized guidance to ensure fellows secure and rewarding job placements after completing their training.
Core Curriculum Lecture Series (Mondays)
This is a weekly conference given by faculty that provides a comprehensive, in-depth review of important aspects in renal physiology, pathophysiology and transplantation that spans 24 months. The conference series includes a two-month orientation session followed by a 4-8-week block of related lectures that concludes with a fellow-directed NephSAP.
Journal Club (Wednesdays)
This is a monthly series directed by our epidemiologist, Dr. Lindsay Kohler, and given by the fellow, focusing on interpreting and critiquing the medical literature.
Clinical Case Conference (Wednesdays)
A monthly case-based conference given by the fellow under the mentorship of faculty, focusing on clinical reasoning incorporating critical elements for diagnosis and an evidence-based approach for management of renal-related diseases.
Pathology Conference (Wednesdays)
A monthly case-based conference given by the fellow and our nephropathologist, Dr. Erika Bracamonte, focusing on in-depth review of renal pathology.
Morbidity and Mortality Conference (Wednesdays)
This is a quarterly conference that focuses on identifying systems-based problems leading to potential adverse outcomes, discussing solutions and implementing action plans to remediate identified problems.
Renal Research Lecture Series (Wednesday)
This is a monthly series that focuses on basic science, clinical research and clinical-based discussions given by divisional, intra- and extramural departmental faculty, and visiting guest lecturers.
Nephropathology Multi-headed Microscope Rounds (Fridays)
This is a bimonthly conference led by our nephropathologist, Dr. Erika Bracamonte, focusing on in-depth biopsy review of native kidney biopsies (second Friday) alternating with transplant kidney biopsies (fourth Friday).
Monthly Board Question Review (Fridays)
Fellows meet with a faculty facilitator and participate in board review questions. The sessions focus on reinforcing knowledge, clinical reasoning and test-taking strategies.
Fellow Housekeeping Meeting
Fellows meet with the program director monthly to review service-related issues, deliver updates and discuss any current issues that impact fellow training. Strategies to promote work-life balance are reinforced during these meetings.
Departmental Conferences
- Weekly Internal Medicine Grand Rounds (Wednesdays)
- Monthly Department of Medicine Research Lecture Series (second Thursday of month)
National Conference Attendance
First-year fellows have the opportunity and receive support to attend the Spring NKF conference. Second-year fellows receive support to attend the ASN conference. Fellows will have additional opportunities to attend national and regional conferences during their fellowship training including Southwest Nephrology Conference, Home Dialysis University and more.
All fellows are expected to participate in a research project during their fellowship. First-year fellows are matched with research mentors in clinical, translational or basic science research. Fellows’ participation ideally culminates in submission of an abstract to one of our national conferences and/or manuscript to a peer-reviewed journal. Fellows additionally participate in quality-improvement projects and may also choose to participate in medical education research. An additional year is available for those trainees interested in more in-depth research exposure.
- Banner – University Medical Center Tucson, 1625 N. Campbell Ave., Tucson, AZ 85719
- Banner – University Medical Center South, 2800 E. Ajo Way, Tucson, AZ 85714
- Southern Arizona VA Health Care System, 3601 S. 6th Ave., Tucson, AZ 85723
- Dialysis Clinic Inc. (DCI) clinics in the greater Tucson area
- Southwest Kidney Vascular Access Center Tucson
- BIO5 Institute
PGY-5
PGY-4
| Name | Graduation Year | Previous Education |
| Hasan Tahsin Ozpolat, MD | 2025 | MD: Istanbul University, Istanbul School of Medicine, Turkey, 2007 Residency: Istanbul University, Istanbul School of Medicine, Turkey, Internal Medicine - General, 2007-2012 Postdoctoral Research Fellow: Lopez Laboratory, Bloodworks Northwest Research Institute, Seattle, 2012-2018 |
| Mohamad Akeel Al-Mula Hwaish, MBBS | 2025 | MD: RAK College of Medical Sciences, Ras Al-Khaimah, United Arab Emirates, 2015 Residency: Tawam Hospital, Al Ain, UAE, Internal Medicine - General, 2016-2020 Residency: University of Arizona College of Medicine – Tucson, Internal Medicine, 2025- |
| Ali Riza Koksal, MD | 2025 | MD: Ondokuz Mayis University School of Medicine, Atakum/Samsun, Turkey, 2001 Residency: Ondokuz Mayis University School of Medicine, Internal Medicine - General, 2003-2008 |
| Nidhi Gupta, MD | 2024 | MD: M.S. Ramaiah Medical College, Bangalore, Karnataka, India Residency: UPMC Medical Education Program, Pittsburgh, Internal Medicine - General |
| Jessica Maria Nino, MD | 2024 | MD: Universidad de Boyacá Facultad de Ciencias de la Salud, Tunja, Colombia Residency: Lincoln Medical and Mental Health Center Program, The Bronx, New York, Internal Medicine - General |
| Shilpa Pedapati, MD | 2024 | MD: Government Medical College, Anantapur, India, 2010 Residency: Guthrie-Robert Packer Hospital in Sayre, Pennsylvania, Internal Medicine, 2018 |
| Srilekha Sridhara, MD | 2024 | MD: Government Medical College Anantapur, India Residency: St Luke’s Hospital Program, Internal Medicine - General, 2010-2013 |
| Asma Rashid, MBBS, MPH | 2023 | MBBS: King Edward Medical University - Lahore, Pakistan, 2011 Residency: Eastern Idaho Regional Medical Center, Idaho Falls, 2021 |
| Preethi Subramanian, MD | 2023 | MD: Sikkim Manipal Institute of Medical Sciences, Gangtok, India, 2009 Residency: Saint Francis Hospital Evanston, Internal Medicine, 2014 |
| Bei Xiong, MD | 2023 | MD: Ross University School of Medicine, 2017 Residency: Coney Island Hospital Internal Medicine, Brooklyn, New York, 2021 |
| Vincent Campion, MD | 2022 | MD: Ross University School of Medicine - Bridgetown, Barbados, 2016 Residency: Lincoln Medical Center, Internal Medicine, 2020 |
| Elvira Gonzalez Negrete, MD | 2022 | MD: Universidad Autónoma de Guadalajara, Mexico, 2010 Residency: ISSSTE Hospital General Dr. Fernando Quiroz, Mexico City, Internal Medicine, 2013 |
| Waseem Albasha, MD | 2021 | MD: University of Arizona College of Medicine – Tucson, 2016 Residency: University of Arizona College of Medicine – Phoenix, 2019 |
| Golnaz Vahdani, MD, MPH | 2021 | MD: University of Debrecen Medical School and Health Science Centre, Hungary, 2012 Residency: Cleveland Clinic, Ohio, Internal Medicine, 2013 |
| Wina P. Yousman, MD | 2021 | MD: Unversitas Padjadjaran Fakultas Kedokteran, Indonesia, 2010 Residency: LAC-USC Medical Center, Internal Medicine, Los Angeles, 2019 |
| Saeed Bidar, MD | 2020 | MD: Tehran University of Medical Sciences School of Medicine, Iran, 1999 Residency: Lutheran Medical Center, Brooklyn, New York, Internal Medicine, 2004 |
| Sevag C. Boyadjian, DO | 2020 | DO: Arizona College of Osteopathic Medicine of Midwestern University Residency: Canyon Vista Medical Center, Internal Medicine, Sierra Vista, Arizona, 2018 |
| Wei Xiang Wong, MD | 2020 | MD: First Moscow State Medical University Named After I.M. Sechenov, Russian Federation, 2011 Residency: University of Arizona College of Medicine – Tucson (South Campus), Internal Medicine, 2018 |
Clinical Services and Rotations
University General Nephrology Consult Service
The University General Nephrology Consult Service operates exclusively as a consultative program based at Banner – University Medical Center, our clinical partner. This 649-bed tertiary care and Level 1 trauma center serves as a key training site for fellows. During their first year of clinical training, fellows dedicate three months to this service, followed by an additional 1 to 1.5 months in their second year.
The consult team manages a dynamic workload, typically handling 10-20 new consults each week while maintaining a patient roster of 10-22 individuals. To ensure ample teaching time for fellows, a patient cap of 22 has been set, supported by an Advanced Practice Provider (APP) offloading service.
Clinical Responsibilities and Skill Development
Fellows take a hands-on role in overseeing the daily management and diagnostic evaluation of all patients under the service’s care. Through this experience, they gain practical expertise in managing a wide range of conditions, including:
- Acid-base and electrolyte disorders
- Acute and chronic kidney disease
- Glomerulonephritis
- Care of hospitalized patients with end-stage renal disease (ESRD)
- Other renal-related conditions
Fellows also develop proficiency in critical procedures and decision-making, such as initiating dialysis, selecting modalities, prescribing treatments for acute kidney injury, placing temporary hemodialysis catheters, and applying principles of urgent-start peritoneal dialysis (PD), including patient selection.
Teaching Opportunities
This service provides an exceptional platform for fellows to mentor and educate resident and student trainees who actively participate in the consult team. The program places a strong emphasis on refining fellows’ teaching abilities, making the consult service an ideal environment to engage with a diverse group of learners and enhance their instructional skills.
University ICU Consult Service
The University ICU Consult Service is based at Banner – University Medical Center, Southern Arizona’s only Level 1 trauma center serving both adult and pediatric patients. Fellows spend 2 to 2.5 months during their first year of clinical training and an additional two months in their second year at this premier facility.
The ICU consult team manages a robust caseload, typically seeing 8-16 new consults per week while overseeing a patient roster of 8-20 individuals.
Dynamic Clinical Experience
This fast-paced, high-energy service immerses fellows in a multidisciplinary environment, collaborating with experts across medical, surgical, trauma, and cardiac ICU settings, which collectively offer over 60 ICU beds. Fellows sharpen their skills in diagnosing and managing complex conditions, including:
- Acute kidney injury (AKI)
- Intoxications
- Placement of temporary hemodialysis catheters
- Selection and management of dialysis modalities, such as continuous renal replacement therapy (CRRT), intermittent dialysis, and prolonged intermittent renal replacement therapy (PIRRT)
Fellows also gain valuable exposure to advanced technologies, including extracorporeal life support (ECLS/ECMO) and cardiac device therapies like left ventricular assist devices (LVAD), total artificial hearts, and other mechanical circulatory support systems, particularly in patients with acute and chronic renal disease.
Focus on Collaboration and Communication
This rotation emphasizes the importance of effective consultative communication and teamwork in a multidisciplinary setting, equipping fellows with the skills to thrive in critical care environments while delivering exceptional patient care.
University ICU Consult Service
The University ICU Consult Service is based at Banner – University Medical Center, Southern Arizona’s only Level 1 trauma center serving both adult and pediatric patients. Fellows spend 2 to 2.5 months during their first year of clinical training and an additional two months in their second year at this premier facility.
The ICU consult team manages a robust caseload, typically seeing 8-16 new consults per week while overseeing a patient roster of 8-20 individuals.
Dynamic Clinical Experience
This fast-paced, high-energy service immerses fellows in a multidisciplinary environment, collaborating with experts across medical, surgical, trauma, and cardiac ICU settings, which collectively offer over 60 ICU beds. Fellows sharpen their skills in diagnosing and managing complex conditions, including:
- Acute kidney injury (AKI)
- Intoxications
- Placement of temporary hemodialysis catheters
- Selection and management of dialysis modalities, such as continuous renal replacement therapy (CRRT), intermittent dialysis, and prolonged intermittent renal replacement therapy (PIRRT)
Fellows also gain valuable exposure to advanced technologies, including extracorporeal life support (ECLS/ECMO) and cardiac device therapies like left ventricular assist devices (LVAD), total artificial hearts, and other mechanical circulatory support systems, particularly in patients with acute and chronic renal disease.
Focus on Collaboration and Communication
This rotation emphasizes the importance of effective consultative communication and teamwork in a multidisciplinary setting, equipping fellows with the skills to thrive in critical care environments while delivering exceptional patient care.
The Transplantation Service operates out of Banner – University Medical Center, functioning as a consultative program in close partnership with the abdominal transplant surgery team. This center is a hub for kidney and kidney-pancreas transplants, having completed over 120 procedures in the past year. Fellows dedicate approximately 4-5 months of their two-year clinical training to this service, which includes both inpatient consultative duties and an outpatient ambulatory component.
Comprehensive Transplant Expertise
During this rotation, fellows gain in-depth knowledge and hands-on experience in key areas of transplantation, including:
- Indications and potential complications of transplantation
- Principles of histocompatibility testing for donor kidney selection
- Psychosocial evaluation and the broader impact of transplantation
- Pharmacology of immunosuppressive drug regimens and their complications
- Workup and management of allograft dysfunction, such as cellular and antibody-mediated rejection
- Recurrence of primary disease
- Immediate postoperative care of transplant patients
Fellows actively participate in the multidisciplinary selection committee, learning the intricate process of evaluating candidates for both living and deceased donor transplants. They also develop a strong foundation in managing the complexities of transplant patient care.
Broader Consultative Role
Beyond kidney transplantation, fellows provide inpatient consultative care to patients with non-renal solid organ transplants—such as liver, lung, and heart—addressing acute and chronic renal disease in these populations. This multidisciplinary approach enhances their ability to navigate diverse clinical scenarios and deliver specialized care.
Dialysis Program
Our Dialysis Program encompasses a comprehensive approach, featuring an acute in-center hemodialysis unit at Banner – University Medical Center (licensed for up to 12 outpatients) alongside an outpatient in-center and home dialysis program tailored for patients with end-stage renal disease (ESRD).
Clinical Training and Exposure
Fellows dedicate six months over two years to this program, participating in outpatient dialysis rounds. They gain hands-on experience in:
- In-Center Hemodialysis: Through partnerships with Dialysis Clinic, Inc. (DCI)—the largest nonprofit dialysis organization—and the Southern Arizona VA Healthcare System, fellows work in outpatient dialysis clinics. They also encounter nocturnal in-center hemodialysis, a rare regional offering.
- Multidisciplinary Care: Fellows collaborate with nursing staff, dieticians, and social workers to deliver holistic patient care.
- Quality and Leadership: Exposure to quality assessment, performance improvement, and the medical director’s role equips fellows with a deeper understanding of dialysis unit operations.
Home Dialysis Focus
Our home dialysis program includes peritoneal dialysis (PD) and home hemodialysis (short daily dialysis), currently serving over 50 patients. We’re expanding this population through initiatives like our urgent-start PD program, designed to enhance growth and honor patient preferences. For broader exposure, fellows can opt for an elective rotation in Phoenix with community nephrologists’ clinics managing over 100 PD patients. Recognizing home therapies as the preferred modality for many, we prioritize training in this area.
Interventional Nephrology Access Center
Fellows also rotate through our interventional nephrology access center, where they master critical skills, including:
- Physical examination and ultrasound of vascular access
- Fistulography and revascularization techniques
- Tunneled dialysis catheter placement and removal
This rotation provides a thorough understanding of vascular access management, a vital component of dialysis care.
Elective rotations are taken during the outpatient dialysis experience. These include but are not limited to renal pathology, rotation in the histocompatibility lab, PD elective with our community nephrology clinics in Phoenix, interventional nephrology and ambulatory clinics. Our program is open to additional elective experiences designed by the fellow and attending faculty together.
The fellow will also be exposed to research in either translational or clinical/population and is expected to participate in a longitudinal project with their research mentor.
Continuity Clinic
The fellow spends one half-day per week in a longitudinal continuity clinic during the course of their fellowship. The patient population comprises a good mix of patient demographics including a large cohort of Latinx and Native American patients. The fellow will become adept at managing CKD, hypertension, glomerulonephritis, stones and long-term post-transplant patients (kidney and non-renal solid organ transplant). We encourage the fellow to take total ownership of their patient panel and the clinic is designed to have two fellows paired with two clinic faculty to promote continuity.
Other Subspecialty Clinics
Fellows can choose to spend elective time in additional transplant clinics including recipient and donor evaluation and post-transplant clinic. Fellows additionally rotate through our multidisciplinary stone clinic staffed by nephrology, urology and nutritional support. We expect to open a glomerulonephritis clinic in 2026.
Leadership
Training in Tucson
How to Apply
Candidates are selected using the following prerequisites and criteria:
- successful completion of an ACGME-accredited residency in internal medicine
- scores on training examinations
- letters of reference
- scholarly accomplishments
The goal is to prepare the trainee to function as a competent nephrologist and meet the requirements for ABIM certification in nephrology.
Your ERAS application will require the following documentation:
- CV
- Three letters of reference
- USMLE scores
- ECFMG certificate (see International Medical Graduates, below)
- Medical school transcript
- Certificate of completion (or good standing in) ACGME-accredited residency
- Personal statement
Please note, you must apply through ERAS and register for participation in the match through the NRMP Fellowship Medical Specialties Matching Program.
International Medical Graduates
Graduates of foreign medical schools are welcome to apply to the fellowship provided they have a standard ECFMG Certificate and an Arizona postgraduate training permit. Fellows must either have U.S. citizenship, valid U.S. residency or a J-1 visa. H1-B visas are supported on a case-by-case basis.
Timeline and Deadlines
The ERAS and NRMP websites have information for fellowship application and match registration deadlines. It is generally recommended applicants start gathering application materials in January to be ready to apply by July. It is highly recommended you have taken Step 3 (pre-boards residency exam). ERAS begins transmitting applications to the fellowship programs in early to mid-July. It is highly recommended your application be completed and submitted by this point. The application review process starts the last week of July through August. Interview offers go out shortly after the review process. Interviews occur over a 6-8 week period beginning the last week of August through October (this may vary depending on the application deadlines for ERAS and NRMP). Rank lists are due in mid-November and the match announcement is in early December.
A fellow accepts employment with Banner University Medical Center as a clinical assistant with designated campus colleague (DCC) status with the University of Arizona.
Research is key to our mission to be a center of excellence for translational research.

Learn more about the residency and fellowship programs at the College of Medicine – Tucson.

Applications are listed as the University of Arizona Program for the July application cycle.
Contact
Bersabe Lopez
Program Coordinator Senior
bersabelopez@arizona.edu
520-621-5227



![[Rayan El Hajjar, MD]](/sites/default/files/styles/az_medium/public/2025-09/El-Hajjar_Rayan_NEPH-5-Edit_25_11412.jpg.webp?itok=ZzNHGNm-)