Current Residents & Fellows
Current Residents and Fellows
Deans Scholarships for Residents and Fellows
Residents and fellows pursuing coursework at the University of Arizona can apply for up to $10,000 in scholarship funding. This program is intended to assist physicians pursuing educational coursework and residency training. Awardees can receive up to $5,000 per semester for a maximum of $10,000 award. Applicants must be employed by Banner Health and pursuing coursework (online or traditional) at the University of Arizona. Their employment must be expected to continue for six months or more at the time of application. The Dean’s Scholarship for Residents and Fellows is a competitive scholarship. Preference will be given to applicants enrolled in UA Health Sciences courses directly aligned with their professional career goals. Applicants will be asked to describe how the course(s) will further their career goals. For more information about the application process, contact the GME office at com-gme@arizona.edu
Trainees participate in a Graduate Medical Education (GME) program sponsored by the University of Arizona College of Medicine – Tucson or College of Medicine – Phoenix. While participating in the training program, trainees are employed by Banner – University Medical Group (B-UMG) and are afforded the opportunity to practice medicine under specified conditions for a designated period of time.
While participating in a training program, trainees are afforded the procedural rights described in the file below.
Residents and fellows are important in the development and education of medical students and their participation at all of our partner institutions is valued deeply.
Clerkships
Residents and fellows must be familiar with the College of Medicine – Tucson specific clerkship learning objectives. These can be found in the syllabus for each clerkship listed below.
- Ambulatory Medicine
- Medicine Inpatient
- Neurology
- Obstetrics & Gynecology
- Pediatric
- Psychiatry
- Surgery
- Family & Community Medicine
- Integrated Emergency Medicine & Critical Care
All clerkship syllabuses were updated February 3, 2026.
Development of Resident Teaching Skills
Residents benefit from additional instruction on how best to teach students. This is addressed at the College of Medicine – Tucson in several different ways:
- In-person sessions sponsored by the College of Medicine – Tucson onsite or elsewhere at other teaching sites
- Sessions that exist as part of their residency program curriculum. Residency programs submit this information annually so the college can assure that all residents are receiving training
- College of Medicine – Tucson web-based residents as educators training is provided each year during onboarding and when residents/fellows advance each year
Drs. Antonino Di Franco and Bjorn Refdors: “Conducting Systematic Reviews and Meta-Analysis” - January 18, 2024
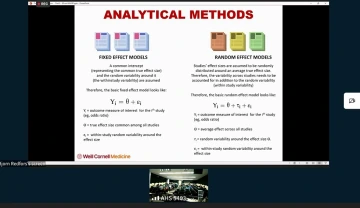
(Click Image to watch video)
Dr. Bonnie LaFleur: “Introduction to Biostatistics and Survival Analysis” and Christine Melton Lopez, “IRB 101” - March 7, 2024
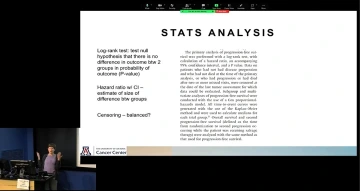
(Click Image to watch video)
Research 101
There is a lot of clinical research-related education available online. The following primer was written by Dr. Spencer Moore, ophthalmology resident and co-director of education for the GME Research Committee.
Study Types
Chronicity
Retrospective: the entire event being studied started, took place, and was completed in the past
Cross-sectional: only a single point in time
Prospective: recruit subjects in present and follow longitudinally over time
Groups
Single-armed: only 1 group (e.g., people who smoke)
Double-armed: multiple groups studied (e.g., control/placebo arm and intervention/exposure arm)
Intervention
None/observational: subjects are studied for the association between an independent variable (e.g., smoking status) and dependent variable/outcome (e.g., development of lung cancer)
Interventional: subjects are grouped according to some treatment or intervention received
Masking
Single-masked: subjects are masked to the status of treatment vs. placebo
Double-masked: subjects are masked to the status of treatment vs. placebo AND investigator is masked to subjects’ group assignment
Randomization
Only possible for prospective interventional cohort studies; avoids selection and allocation biases inherent to nonrandomized study design. Allows for evidence of causality between independent (e.g., treatment/intervention) and dependent (e.g., outcome) variables.
Elements of Research Proposal
A well-referenced and concise written research proposal is essential. Depending on where you are sending it (UA RIA, UA IRB, SAVAHCS, Banner, private funding agencies, etc.), there may be differences in the format. In general, the format will include the following elements:
Abstract
May or may not be included depending on format. It should be 1 paragraph and about 250-300 words long. It would include a brief few sentences of background and introduction. This should lead into the knowledge gap in the field and set up the reader for the hypothesis to be tested. Next, the study design and aims should be stated as briefly and concisely as possible. Next, the hypothesis should be stated, followed by the importance or significance of potential results in the field. The abstract generally does not contain references.
Background & Introduction
Should be about 1 page or less of single-spaced background and introduction to the topic being studied, usually for a general medical or scientific audience. This section should be well referenced. Introduce the condition being studied and some of its public health implications. Then describe what is known in the field about your specific topic. This should progress logically toward the question your study seeks to answer. You may conclude this section with something to the effect of, “In the present study, we plan to use [insert study design here] to answer the question of [insert major research question or knowledge gap here].”
Specific Aims
Depending on the format of the study, this may be a single aim with several sub-aims, or multiple specific aims, each with their own sub-aim. Describe the format of the study, the patient population to be studied, means of recruitment, data points to be collected, type of statistical analysis and comparisons to be performed. Include a testable hypothesis related to the aim described. Each aim should be about 1 paragraph.
Protocol
This will include a detailed account of the experimental protocol. It may be several pages long. It will vary according to your specific project. Organize it according to each specific aim. It will include a detailed description of the patient population being studied, how those patients will be selected or recruited, the source of data to be collected, the data points that you will collect and how those data will be analyzed. You should also include a selection relating to human subjects protection that describes how clinical data will be safeguarded, how human subject identities will be protected and deidentified, how data will be stored, etc. If subjects are being actively recruited and consented for a study there will be an additional section describing the informed consent process and how subjects will be recruited. Include a primary outcome measure in your data to be collected and a description of how this will be calculated. For example a primary outcome measure in a prospective observational cohort study of smokers and nonsmokers might be the development of lung cancer within 10 years, and the statistical analysis to be performed might be relative risk of developing lung cancer within 10 years of enrollment. If there is any prospective component to your research component, where patients are brought in for testing or treatment, then you will need to identify a funding source — your research mentor can assist you.
Power Analysis
For a prospective study, it is important to have some statistical basis to calculate the number of subjects you plan to recruit. For a retrospective study, this can also be helpful to determine the number of charts needed to review. There are various online sample size calculators as part of your power analysis.
Statistics
It is important to have a reasonable grasp of statistics in your research protocol. Understand exactly what clinical data will be collected so that you can propose the appropriate statistical analysis.
Some common statistical tests:
t test: to compare means of 2 groups with continuous numerical data. Generally, it would be a 2-tailed, unpaired t-test. For example, you could compare the mean age of 2 groups.
Chi-square or Fisher exact test: compares the proportions of 2 subjects in 2 groups. For example, you could compare the percentage of subjects in 2 groups who develop lung cancer.
ANOVA: to compare group means of a dependent variable with multiple different levels of the independent variable, for example systolic blood pressure levels with different dosages of blood pressure medications.
Kaplan Meier: comparing survival or latency to meet some primary outcome measure over time. Can calculate a Kaplan Meier or log-rank statistic to compare survival in 2 different groups.
Tips
You will probably need 2 separate and parallel research applications approved before starting your project if using the UA research infrastructure and IRB. Your department likely has research coordinators who can help you and determine any documents you will need. This will probably include approvals from the Research Intake Application (RIA) and an Institutional Review Board (IRB).
UA REDCap is a great secure way to store clinical data. If you will be collecting lots of separate data points, REDCap is an efficient way to store, organize and sort data that can easily be anonymized and exported.
Step by Step: Conducting Research
Conducting research as a trainee can be daunting. Consider the following steps to get you started with conducting a human research project, and please also discuss with your mentor. For an explanation of the full IRB process, review the “Getting Started” webpage at RII.
Seven Steps to Conducting Research
Complete CITI Human Subjects Protection training
Complete the Biomedical Research BASIC Course at CITI Program.
Download IRB forms
Download the appropriate forms from the IRB website:
- IRB protocol
- consent forms
- applicable appendices
- attestations from your adviser, scientific reviewer, and department head
Begin eIRB submission
Begin your submission at the eIRB website (NetID required). This how-to video may help you to complete this step.
If applicable, submit to Banner
If Banner staff, patients, medical records or specimens will be used, submit your study through the Research Administration Portal (RAP) (NetID required).
Add Banner approval to eIRB
Once RAP is approved, add the approval email to your study in eIRB and press “Submit” for your IRB to be formally submitted. An IRB coordinator will be assigned to pre-review your study prior to final IRB chair review/approval. Anticipate receiving comments and questions for further revision during this phase. Once the study is approved, you will receive an eIRB system-generated email. Make sure to review your approval letter to understand reporting requirements moving forward. You can then begin your research.
Work with statistician
Once the data from the project is available for analysis, work with a statistician to help with the pre-defined statistical analysis plan, and interpret the results to draw meaningful conclusions related to the research question.
Share your results
Consider presenting your research at local and or national meetings, as you are collecting your data with the ultimate goal of a peer-reviewed manuscript publication.
Please type keywords into UA Profiles to identify a mentor with similar research interests.
Resident and Fellow Academic Support Services
Individual Appointments for Residents and Fellows For:
- In-training exams
- Specialty and subspeciality board exams
- USMLE Step 3/COMLEX-USA Level 3
- Test-taking strategies
- Retention challenges
- Learning strategies
- Study schedules
- Pre-rounding efficiency
- Time management and efficiency issues (for studying)
- Integrating feedback and effectively asking for feedback
Schedule an appointment with RoseMarie Smith, GME learning specialist.
Workshop Topics Available for Request:
Coaching and advising can help empower your journey. Take the first step today and plan your strategy session.
- Create a personalized study plan for board studying (specialty- or subspecialty-specific requests)
- Setting realistic study goals for your ITE and beyond
- Myths of learning styles and tips for learning
- Strategies for using a question bank
- Learning strategies and test-taking tips
- Learning strategies/recommendations for professional reading
- Effectively asking for feedback
- Using feedback
- Other workshops available upon request
Program directors, program administrators and chief residents can request a workshop. Please e-mail the GME learning specialist directly.
USMLE Step 3 is the final exam in the USMLE sequence. USMLE Step 3 is different than previous USMLE exams you have taken. First and foremost, this exam is divided into two separate days and the second day includes not only multiple-choice questions but also case simulations. Additionally, you are now in residency and do not have dedicated time to study for this exam and will need to adopt a tailored approach for studying for this specific exam.
The first step to take in preparing for Step 3 is to develop a timeline of when you will take the exam and how much time you have to prepare. Most residents end up using these three resources to study for Step 3: UWorld Question Bank, Master the Boards USMLE Step 3, and OnlineMedEd. OnlineMedEd is free and contains many high-yield videos. Typically for Step 3, the intern contact is valuable as well as the corresponding subjects that are not covered in the intern’s specialty. For example, pediatric residents can benefit from a cardiology refresher video.
If you would like further assistance on Step 3 and how you might create a study plan, please make an appointment with the GME Learning Specialist RoseMarie Smith.
For more information on the content and formatting of the exam, visit the USMLE Step 3 webpage. To take Step 3, you need to submit an application on the Federation of State Medical Boards.
COMLEX-USA Level 3 is the final exam in the COMLEX sequence. Candidates take COMLEX Level 3 after graduating from their doctor of osteopathic school. COMLEX Level 3 is different than previous COMLEX exams you have taken. This exam is the most challenging and takes two separate days to complete. There are multiple choice questions and also clinical decision-making cases. Additionally, you are now in residency and do not have dedicated time to study for this exam and will need to adopt a tailored approach for studying for this specific exam.
The first step to take in preparing for COMLEX Level 3 is to develop a timeline of when you will take the exam and how much time you have to prepare. Residents usually use one of two questions banks, either COMBANK from TrueLearn or COMQUEST. Then they also use an osteopathic medicine book such as OMT Review: A Comprehensive Review in Osteopathic Medicine. One advantage of selecting to use COMBANK (from TrueLearn) is you can add a predictive assessment exam to your question bank for an additional fee.
If you need to refresh your memory on certain topics you might want to check out OnlineMedEd. This resource is free and contains many high-yield videos. Typically for Step 3, the intern contact is valuable as well as the corresponding subjects that are not covered in the intern’s specialty. For example, pediatric residents can benefit from a cardiology refresher video.
If you would like further assistance on COMLEX Level 3 and how you might create a study plan, please make an appointment with the GME Learning Specialist RoseMarie Smith.
For more information on the content, exam format and registration visit the NBOME webpage.
As you embark on searching for an attending position after residency or are applying to a fellowship, you want a well-polished curriculum vitae and to be ready for interviewing at any time.
Cover Letter Tips
Not all jobs require a cover letter but when they do, a well-written cover letter can help you stand out from the other applicants. Your goal in a cover letter is to prove you are exactly what the employer is looking for and you want to answer these three questions:
- Why are you interested in the position?
- How are you qualified for the position?
- Why are you a good fit for this position?
Curriculum Vitae (CV) Tips
A curriculum vitae is meant to document your entire academic history and work history. Here are few tips:
- Include your name, credential, specialty or subspecialty, and contact information in your heading
- To make your application more cohesive, use the same font type on all parts of your CV, as well as your cover letter, research statement, reference list, etc.
- Provide your name in a footer or header on every page of your CV, as well as other application materials
- Do not include your SSN, age, gender, race, religion, political affiliation, marital/parental status, disability or national origin, or DEA numbers
Learn more from the AAMC and the AMA.
- Dress accordingly: Interviews are formal, so you should be too.
- Do your research on the fellowship or hospital, department and division you are applying to. Use the webpages and see if you can find any specific strengths, weaknesses or unique aspects. This shows the program or place you are interviewing with that you have done your homework.
- Avoid generic answers for questions. Instead, make an impression and give succinct answers with examples.
- Practice, practice, practice: Practice alone or with someone else, which will reduce embarrassment, help refine your answers, and help you be far more relaxed on interview day.
- Prepare questions ahead of time: Asking questions shows your interest in the fellowship or position you are applying for.
- Show gratitude by sending a thank you note: It is appropriate to send a thank you email after interviewing within 24 hours. A thank you note should include key parts to your conversation, reiterate interest in the program or position, and invite a request for additional information or follow-up.
Frequently Asked Questions
All appointments are provided free of charge to all residents and fellows.
Residents and fellows visit for various reasons: to learn more efficient ways of studying, develop an effective study plan, explore test-taking strategies, edit a statement for a fellowship, figure out a pre-rounding strategy, and more. Regardless of why you would like to meet, any resident or fellow is welcome to make an appointment.
It is helpful to have a general idea of what you would like to focus on (study plan for an in-training exam, pre-rounding efficiency, etc.). During our first meeting, you will be asked about your background, and you and the specialist will discuss your past and current strategies for learning and other information as relevant. Finally, you will get into why you made the appointment in the first place, so it is always a good idea to know what you hope to take away from the appointment.
Most appointments are voluntary and stay between you and the GME learning specialist. However, in some situations if your program required you to make a meeting (e.g., for an ITE referral), meeting dates, a general summary of the meeting, and recommendations will be shared with program personnel. If there is something you would not like shared with your program, be sure to let the GME learning specialist know when you meet.
Contact RoseMarie Smith to schedule, change or cancel your appointment. Please notify the office 24 hours in advance of a cancelation, allowing us to use the time for other residents or fellows in need.
RoseMarie Smith, MA
Resident and Fellow Learning Specialist
Certified School Psychologist
Educational Consultant
Behavior Specialist
psychedintegrated@gmail.com
520-433-1544
Please notify RoseMarie Smith at psychedintegrated@gmail.com if you will be late or need to cancel or reschedule your appointment. Twenty-four-hour notice of cancellation allows us to use the time for other residents or fellows in need.
Accommodations are not handled by the GME learning specialist. Instead, there is a specific process to follow. Trainees with qualifying disabilities who require accommodation within their training program should contact the university’s Disability Resource Center (DRC) at 520-621-3268 or drc-info@arizona.edu. More information is available at https://drc.arizona.edu. Accommodations to the physical workplace will be coordinated through the DRC along with Banner Human Resources. Trainees are responsible for initiating the accommodation process.

