Department of Medicine
Internal Medicine
Internal Medicine Residency Program – Tucson
Since 1972, we’ve graduated hundreds of physicians trained in all aspects of primary care. Residents learn the fundamentals of inpatient medicine while caring for patients on the general medical wards and in state-of-the-art intensive care and cardiac care units, with ample exposure to ambulatory medicine. We also enjoy one of Arizona’s highest board passage rates.
We also offer access to multiple affiliated Centers of Excellence, including the University of Arizona Cancer Center, Sarver Heart Center, Asthma and Airway Disease Research Center, Arizona Arthritis Center, Arizona Center on Aging, Center for Disparities in Diabetes, Obesity, and Metabolism, Thomas D. Boyer Liver Institute and the BIO5 Institute. Faculty welcome our residents into their laboratories to participate in both clinical and bench research. As a result of our rigorous clinical and scientific training, our program has a history of matching its graduates into competitive fellowships and careers.
If you are looking for a highly collegial, mid-sized academic training program that offers diverse experiences at multiple state-of-the-art training sites, with high academic standards and rigorous clinical models, we welcome you to visit and meet our leadership, faculty and residents as part of our interview process. Come grow with us!
About Our Program
Conferences
To promote housestaff education, a number of required conferences are scheduled during the work week. These include Noon Conferences, our Thursday Academic Half Day for all residents, as well as Morbidity and Mortality Conference sessions and Medicine Grand Rounds held weekly at each hospital. Residents on the inpatient service also participate in bedside attending rounds. Each institution is staffed using a teacher/hospitalist attending model, whereby each team is managed by one attending.
Call Schedule
While in training, call schedules vary by institution. At Banner University Medical Center – Tucson (B-UMCT), code pager duty is every fifth day on the general medicine wards. While on CCU, call is every fifth night with a senior resident in-house and dedicated to assisting interns assigned to call. ICU call is variable, occurring every fourth or sixth night. At the Southern Arizona Veterans Affairs Health Care System (SAVAHCS), long call is every third day. Interns and residents are assigned several weeks in the course of the year where they may be called in for jeopardy in the event that a colleague suffers an illness or other personal or family emergency. There is no 24-hour call for interns.
Ambulatory Experience
Our ambulatory training provides the opportunity for residents to establish long-term therapeutic relationships with their patients. Categorical residents participate in continuity clinics throughout all three years of their residency. Clinic sites include South Campus (Banner – UMC South) and Pantano Clinic (Banner – University Medicine Specialty Services Clinic at 22nd and Pantano), VA hospital (SAVAHCS) and a private practice. In our 4+1 system, residents participate in various rotations for four weeks followed by one full week of clinic. Residents only see clinic patients during their clinic weeks. There are no scheduled continuity clinics during wards, ICU or elective rotations. During clinic weeks, each resident will be assigned to five half-day clinic periods. Each resident will follow their individualized clinic schedule throughout the academic year. During clinic weeks, when a resident is not in a clinic to see patients, they have the opportunity to complete patient care tasks, work on quality-improvement projects or participate in an extra subspecialty clinic half-day.
Residents may establish an extra subspecialty clinic half-day with a mentor and participate in this extra subspecialty during every continuity clinic week. All clinics are supervised by attending physicians who offer their guidance and assist with patient management. For additional learning, we use the Johns Hopkins clinic curriculum, which allows residents to work through question-based didactic modules pertinent to outpatient medicine. During their second year, residents also participate in an additional one month of community-based outpatient medicine where they work one-on-one with an experienced private practice internist. In this setting, residents not only gain further experience in outpatient medicine, but also gain exposure to practical issues of billing, coding and clinic management.
Electives
Elective experiences are designed to allow residents to customize their training in accordance with their career plans. Elective options are varied and flexible ranging from internal medicine subspecialties to radiology, pathology, orthopedics and palliative care. In addition, many residents elect to pursue research opportunities.
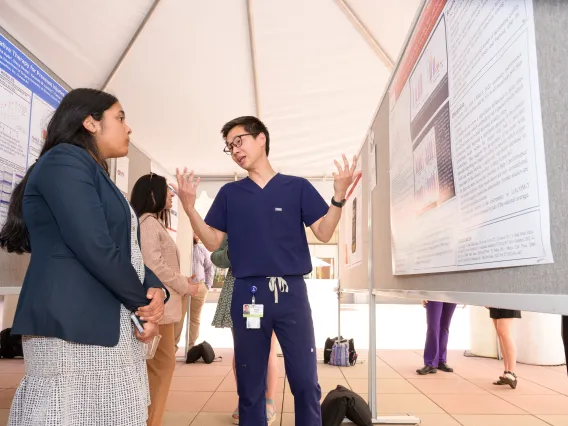
Research
PYG2 or PYG3 residents may elect to do formal research projects with a faculty mentor, ranging from bench to clinical research. Many residents have published abstracts and papers and received grant support. Many residents compete in the American College of Physicians (ACP) Clinical Vignette Competition for the ACP Arizona Chapter Scientific Meeting and are encouraged to submit clinical and research abstracts for this meeting. Residents may also do posters, the oral vignette or Doctor’s Dilemma competitions.
End Result
In all three years of training, an emphasis is placed on the team approach to patient care. At each level, residents are encouraged to learn and teach the important aspects of clinical evaluation and the pathophysiology of disease processes. With each year of additional training, greater responsibility for patient care and teaching of other team members is given. All residents will experience critical care, medical consultation, community-based private practice, ward medicine, electives and continuity clinic. By the completion of the third year, residents are expected to be competent and independent in inpatient and outpatient medicine.
Career Success
Our residents have been fortunate to enter the fellowships and practices of their choice. Recent graduates have entered fellowships at our own institution as well as Banner – University Medical Center Phoenix, Cleveland Clinic, Johns Hopkins, Mayo Clinic, Yale, Stanford University, Brown University, Harvard University, Rush-Presbyterian, University of North Carolina, University of Alabama, University of Cincinnati, University of Virginia, University of Wisconsin, UT Houston, UT San Antonio, Loma Linda University, UC San Diego, Tufts University, Duke, Tulane, Wake Forest, Washington University, UCLA and USC.
Banner – University Medicine
The affiliation with our primary clinical partner began in 2015 with the Arizona Board of Regents-approved merger of the University of Arizona Health Network with Banner Health to create Banner’s academic division, Banner – University Medicine. Banner is one of the largest nonprofit health care systems in the country with 33 acute-care hospitals and health care facilities. With more than 55,000 employees, it’s the leading nonprofit provider of hospital services in all the communities it serves and the largest private employer in Arizona.
Banner – University Medical Center Tucson
1625 N. Campbell Ave., Tucson, AZ 85724
With the opening of this 670,000-square-foot hospital tower in 2019, Banner – UMC Tucson increased its overall licensed hospital beds from 479 to 649. This includes 228 private patient rooms, 20 new and larger operating rooms, and 96 more intensive care adult beds. An entire floor is devoted to labor and delivery (with 12 light-filled labor and delivery suites and 24 maternity rooms) and enhanced telemedicine capabilities throughout. This hospital is the only Level I Trauma Center designated in Southern Arizona. In 2024-25, it was named a U.S. News & World Report Best Regional Hospital, ranking No. 1 in Tucson, No. 3 in Arizona and the best hospital in Southeastern Arizona. It is listed as high-performing in cancer, gastroenterology and GI surgery, geriatrics, pulmonary and lung surgery, and urology.
The hospital also is accredited as a Primary Stroke Center by The Joint Commission, Chest Pain Center by the Society of Cardiovascular Patient Care, Non-Invasive Vascular Lab by the Intersocietal Accreditation Commission (IAC), Comprehensive Cancer Center by the National Cancer Institute, an NPF Referral Center by the National Pancreas Foundation, and a Magnet hospital by the American Nurses’ Credentialing Association. Its Interstitial Lung Disease Program, operated with the University of Arizona Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, also was chosen as a member of the National Pulmonary Fibrosis Foundation’s Care Center Network. Its Petersen Clinics, operated with the University of Arizona Division of Infectious Diseases, are recognized by the University HealthSystem Consortium (predecessor to Vizient) as No. 3 in the nation for HIV patient care. And it is designated as one of 55 Ebola Treatment Centers in the nation by the U.S. Centers for Disease Control and Prevention. Becker’s Hospital Review also named Banner – UMC Tucson one of the “100 Great Hospitals in America.”
Banner – University Medical Center South
2800 E. Ajo Way, Tucson, AZ 85713
With 245 licensed beds, this hospital in South Tucson is recognized as an IBM Watson Health 100 Top Hospital in the U.S. and an Everest Award winner for its rate of improvement in quality care over five years. The facility also is an accredited Cardiac Receiving Center by the Arizona Department of Health Services (ADHS), Non-Invasive Vascular Lab by the IAC, a Certified Diabetes Self-Management Education Program by the American Diabetes Association, an Infectious Disease Treatment Center of Excellence by the ADHS, and a Senior Friendly Hospital by the Nurses Improving Care for Healthsystem Elders (NICHE) Program.
Banner – University Medicine North
3838 N. Campbell Ave., 3838 N. Campbell Ave., Tucson, AZ 85719
This 208,000-square-foot, three-story, state-of-the-art multidisciplinary adult outpatient services center is located on 13 acres, and includes Building 2, nestled between the University of Arizona Cancer Center – North Campus clinic and the Ronald McDonald House of Southern Arizona on Allen Road east of Campbell Avenue. Patient care for the more than 25 specialties range from cardiology to neurosurgery to rheumatology.
University of Arizona Cancer Center – North Campus
3838 N. Campbell Ave., 3838 N. Campbell Ave., Tucson, AZ 85719
This 82,000-square-foot outpatient care facility provides state-of-the-art equipment and highly specialized professionals to diagnose and treat patients. Our multidisciplinary patient-care teams include internationally renowned medical, hematological, radiation and surgical oncologists as well as nurse practitioners, nurse coordinators, research specialists, psychiatrists, social workers, patient advocates, nutritionists, pharmacists and genetic counselors. Its main campus research affiliate, the University of Arizona Cancer Center, received its first support grant from the National Cancer Institute (NCI) in 1978, became an NCI-designated comprehensive cancer center in 1990, and is now one of 45 nationally and remains the only one with headquarters in Arizona. Drawing faculty from 14 academic departments and five colleges, the center has 73 research labs where about 300 physicians and scientists conduct collaborative research. It has developed a range of new cancer treatment and preventive agents and also has spun off more than 15 companies.
Southern Arizona VA Health Care System
3601 S. 6th Ave. Tucson, AZ 85723
The VA Medical Center in Tucson is the flagship facility for the Southern Arizona VA Health Care System (SAVAHCS), which serves over 170,000 veterans in eight counties in Southern Arizona and one county in western New Mexico. This 277-bed hospital provides training, primary care and subspecialty health care for eligible veterans. Programs supported include medicine, surgery, neurology, mental health, geriatrics and advanced rehabilitation. SAVAHCS is home to the nationally recognized Geriatrics and Rehabilitation Center, designated in 1999 as a VHA national center of excellence for geriatrics evaluation and management. It is the principal affiliate of the University of Arizona colleges of medicine, nursing and pharmacy in Tucson. It has affiliations with 70 academic institutions and trains more than 700 physicians, nurses, pharmacists and allied health students a year. The SAVAHCS Research Service supports 70 principal investigators involved in more than 186 research projects in areas such as diabetes, colon cancer, Valley fever, bone cancer, the biochemistry of depression, treatment for heart failure and pulmonary diseases such as asthma and emphysema. The SAVAHCS has increased access for veterans by activating community-based outpatient clinics (CBOCs) in Casa Grande, Green Valley, Safford, Sierra Vista, northwest and southeast Tucson, and Yuma. It also has sharing agreements with Ft. Huachuca and Davis-Monthan Air Force Base to provide health care services for active duty service members. SAVAHCS is a TRICARE and CHAMPVA provider for retirees and eligible family members. Additional sharing agreements exist with Banner – University Medical Center, the Indian Health Service and Tucson Medical Center. SAVAHCS also was designated as a Polytrauma II Center in 2006.
Our 2025-2026 interview season will be held virtually and will begin mid-October 2025 and conclude in February 2026. All applicants must have an NRMP number and an AAMC number to be able to match in any program.
Application Procedure
Positions are offered through the National Resident Matching Program (NRMP). Candidates can access the ERAS program by visiting AAMC FREIDA (program code: 1400321029). Completed applications must be submitted through ERAS and consist of the following:
- Letters of recommendation (LOR), (three minimum, four maximum)
- Curriculum vitae or resume
- Dean’s letter or Medical Student Performance Evaluation (MSPE)
- Medical school transcripts
- Passing scores on USMLE 1 & 2 or COMLEX 1 & 2
- Personal statement
- Proof of graduation
Program Signals: While we generally review applications from those who signal our program first, we also welcome (and routinely interview) applicants who do not signal us. More information about program signals.
Medical Licensing Exams: Although there is no set USMLE or COMLEX cut-off score, applicants should have a strong USMLE Step 1 and Step 2 to be competitive.
- Applicants should have substantial and credible hands-on clinical experience (not observerships) of at least two months in the U.S. within the last three years
- Applicants with USMLE scores must have taken and passed USMLE Step 2 (CK) by the time the program is required to submit our Rank Order List
- Applicants should have graduated from medical school within the last five years
- A typical invited interviewee will be scheduled for a half-day of program presentations, interviews and discussions with housestaff
- All hired interns must pass a background check and will need to pass a pre-employment drug screening
- As a condition of employment, all new residents must obtain a valid fingerprint clearance card, in accordance with A.R.S. 15-1881, and pass a criminal background check.
International Medical School Graduates
- Applicant must have passed USMLE Step 1
- USMLE Step 2 (CK) must be verified before match
- ECFMG must be certified by the start of the program
- Applicant must enter on a J1 Visa — unfortunately, Banner University Medical Center does not sponsor any other visas
We, the members of the Department of Medicine, are embarking on a mission to create, nourish and sustain a residency training curriculum founded on the philosophical ideal of the comprehensive internist.
We believe that the ideal, inclusive, comprehensive internist is characterized as:
- An expert in managing diseases of diverse populations, such as older adolescents and adults, and are equally effective in the office and in the hospital setting.
- A consultant to all populations of patients and generalist physicians — in rural, underrepresented and other special environments — for difficult or undifferentiated patient problems, or in areas in which the internist has a unique expertise.
We also believe that the future comprehensive internist will be:
- A compassionate and ethical physician who is a passionate advocate for equity of all patients.
- A physician who is trained in clinical epidemiology, clinical decision-making and preventive medicine.
- A master of communication, who listens and conveys information effectively, without bias, to patients and colleagues.
- A resource manager who can bring a thoughtful and efficient style of practice to the evaluation and management of diverse patients and their problems.
- A generalist in outlook who possesses special skills to respond to the changing medical and social needs of local communities.
- An effective leader and coordinator of the entire patient care team who can work in a complementary fashion with equality for all members of this team.
- A clinical information manager who can take full advantage of electronically stored data and who can use the most modern technological tools for communication.
- A person who is capable of balancing between personal growth and professional development.
Accordingly, we are committed to designing and developing a curriculum that:
- Offers a solid foundation in the management of patients with complex multi-system disorders, preventive medicine and the delivery of health care.
- Instills a foundation for future training in subspecialty medicine and/or medical research.
- Promotes attributes and skills for life-long learning, inquiry and teaching.
- Develops the skills required to function and excel in multiple practice settings.
- Brings awareness to issues of race, gender, ethnicity, culture, the medically underserved and issues specific to Indigenous peoples.
We recognize that the goals of education and service are correlated and are equally essential for the effective training of future comprehensive internists. Consequently, we are committed to providing our residents with a supportive learning environment that enables them to successfully attain those objectives.
Rotations
The Division of Cardiology believes that a strong knowledge of the fundamentals of cardiovascular disease is critical for every internist, as cardiovascular disease is common and will be managed by all primary care providers and specialists. In the interest of ensuring all our trainees have knowledge of common and complex heart diseases, we sponsor a number of rotations and electives at our primary clinical partners, Banner – University Medical Center (UMC) Tucson and South campus and the Southern Arizona Veterans Affairs Health Care System (SAVAHCS).
Cardiovascular Residency Rotations and Electives
- Coronary Care Unit at Banner – UMC Tucson campus
- Cardiology Consultation Service at Banner – UMC Tucson campus
- Electrophysiology Service at Banner – UMC Tucson campus
- Ambulatory Cardiology Clinics at Banner – University Medicine North campus
- Ambulatory Advanced Heart Failure and Transplant Service at Banner – UMC Tucson and North campuses
- Cardiology Consultation Service at Banner – UMC South campus
- Cardiology Consultation Service at SAVAHCS
A typical rotation for a resident physician in our division might include exposure to:
- Inpatient guidelines-based management of cardiovascular disease
- Cardiac imaging
- Management of arrhythmias and advanced electrophysiology procedures
- Management of advanced heart failure
- Cardiac catheterization, percutaneous and structural interventions
- Cardiothoracic surgery including bypass and valve surgery
- Cardiopulmonary rehabilitation
- Management of mechanical circulatory support devices
- Heart transplant
- ECMO (extracorporeal membrane oxygenation)
The Division of Cardiology firmly believes in fostering interest and feeding the passion of trainees for cardiology. Each year we award the Charles W. Hall Jr. Memorial Award to the Outstanding House Officers on the Coronary Care Unit rotation. Recipients are selected by cardiology faculty and fellows based on their quality of work, attentiveness, decision-making and knowledge.
Internal medicine residents are encouraged to participate in the endocrinology, diabetes and metabolism rotation, which takes place in the diabetes clinic on the third floor of Banner – UMC North, Building 2. The elective is primarily a clinical rotation. The resident will participate in clinic activities, endocrine didactics sessions, tumor board and other special conferences.
During this elective, the resident will have a hands-on experience with patients specifically scheduled for them in a designated resident clinic. The resident will have the opportunity to gain knowledge on health promotion, disease prevention, diagnosis, care and treatment of patients from adolescence to old age. The resident will see patients with a variety of hormonal problems, metabolic bone and mineral disorders and will improve their understanding of the detection, management and treatment of Type 1 and Type 2 diabetes. Along with the attending physician and allied health professionals, the resident will participate in the development of each patient’s plan of care.
Internal medicine residents work with gastroenterology and hepatology faculty in an inpatient and outpatient setting, including at the endoscopy labs at both Banner – UMC Tucson as well as Banner – UMC South and at the Southern Arizona VA Health Care System’s flagship Tucson hospital. They gain additional clinical exposure with the University of Arizona Thomas D. Boyer Liver Institute, which is affiliated with the Division of Gastroenterology and Hepatology.
Residents on a geriatric medicine rotation will spend two to four weeks at both Banner – UMC Tucson on the Geriatrics-Orthopedic Inpatient Consult Service, and at the Southern Arizona VA Health Care System with the Home Based Primary Care program. During this rotation, they also will have opportunities to work with physicians in geriatric rehabilitation, neurogeriatrics, the Fragility Fracture Service Clinic, and ambulatory geriatric medicine clinics.
On a palliative medicine rotation, residents will follow the palliative care team on the inpatient consult service for two weeks. Along with other members of the interdisciplinary team, social workers, case managers and those in the chaplaincy, they will participate in helping patients and families navigate complex decision-making, determine goals of care and complex symptom management.
Chief Resident Immersion Training (CRIT) Program
The Chief Resident Immersion Training (CRIT) in the Care of Older Adults Program, in cooperation with the Association of Directors of Geriatric Academic Programs, is funded by a grant to the University of Arizona Center on Aging, which is directly affiliated with the Division of General Internal Medicine, Geriatrics and Palliative Medicine. The program focuses on providing chief residents — including those at our primary teaching hospitals, Banner – University Medical Center Tucson and South campus — with a combination of training focused on improving their understanding of geriatric principles, including teaching and leadership skills.
Internal medicine residents work with Division of Infectious Diseases faculty in an inpatient and outpatient setting at both Banner – UMC Tucson and Banner – UMC South as well as at the Southern Arizona VA Health Care System’s flagship Tucson Medical Center.
In the infectious diseases rotation, residents learn to manage common infectious disease-related problems. The rotation consists of patient consultations, ward rounds with an attending physician and clinical pharmacologist, clinical conferences and instruction in the central clinical microbiological laboratory. Residents will be provided a core curriculum outline and current literature references. Scheduled events during the rotation will include infectious disease subspecialty noon conferences (monthly at SAVAHCS) and infectious disease conferences weekly at Banner – UMC Tucson.
Inpatient medicine is a core part of medical education and residency training. Our faculty play a major role during rounding in inpatient wards as clinical educators and teachers. We provide supervision in the care of medically complex patients with diverse ethnicities, disease processes and socioeconomic statuses. We also work closely with different subspecialists and surgeons, partnering in the care of post-operative patients, ensuring smooth transitions of care for them and their families.
Currently, we staff the following resident teams:
- Five full teaching teams and one resident-only team at Banner – UMC Tucson
- Two of the three internal medicine teams at Banner – UMC South
- One night-float team at Banner – UMC South and staff two night-teams at Banner – UMC Tucson to support all admissions at night
Our faculty are actively involved in teaching residents by creating innovative rounding strategies, conducting board review courses (five hours per week), guiding residents in developing and conducting QI projects, and teaching them bedside procedures utilizing point-of-care ultrasound.
The Division of Nephrology provides renal electives to internal medicine residents. These electives provide a complete exposure to all aspects of renal medicine from kidney transplantation to palliative care.
Both our residents and medical students are exposed to the following topic areas/procedures:
- Inpatient evaluation of acute kidney injury
- ICU nephrology
- Electrolyte and acid base disorders
- Glomerulonephritis
- Care of the end-stage-renal-disease patient
- Chronic kidney disease treatment and prevention
- Pharmacology dosing for renal function
- End-of-life care
- Nephropathology
- Transplant nephrology
- Transplant surgery (participation in living or deceased donor kidney transplant)
- Renal replacement modalities for the inpatient (continuous and intermittent)
- Outpatient dialysis (in-center hemodialysis and home therapies, both hemodialysis and peritoneal dialysis)
- Urine sediment evaluation
- Didactic conferences three times a week
Internal medicine residents work with Division of Rheumatology faculty primarily in the outpatient setting at Banner – UMC South, Southern Arizona VA Health Care System and the Indian Health Service – Pascua Yaqui clinic.
As part of the team, the medical resident in the outpatient clinics will conduct patient interviews, perform physical examinations and review relevant laboratory data. With the faculty, they will then formulate an assessment and management plan. They will participate in weekly rheumatology conferences (including Grand Rounds, Fellows’ Conference and multidisciplinary conferences), which cover clinical and basic science topics in rheumatology, musculoskeletal radiology, immunology, research study designs and various other topics.
The Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine oversees a two-week rotation in sleep medicine. Residents will learn to diagnose and treat common sleep disorders including insomnia, hypersomnia, sleep-related movement disorders and obstructive sleep apnea, and will understand how to interpret sleep studies and guide patients in CPAP therapy and other treatments.
Curriculum
Presenters are faculty members, offering didactic as well as interactive case-based sessions on topics within the medicine subspecialties as well as interdisciplinary topics important for the training of a well-rounded internal medicine resident. Residents are constantly challenged to apply this material not only in clinical duties, but also during the interactive case- and question-based sessions following the lectures. In addition to the high-quality delivery of didactics, an added bonus is the camaraderie that has become a natural byproduct of these afternoons. You will not only come away with thorough exposure to the subspecialties and a head start toward board preparation, but you will also mingle with your colleagues on a weekly basis, encouraging better work relationships and friendships outside the hospital.
Medicine Grand Rounds
Grand Rounds, except for a summer hiatus between mid-June and mid-August, are held weekly on the fifth floor from noon-1 p.m. on Wednesdays. They are viewable live from main campus or streamed via webcast at other sites.
VA Management Conference
The VA Management Conference is held at the Southern Arizona VA Health Care System on second and fourth Tuesdays, noon to 1 p.m., in the Patio Conference Room.
The following is a sample of didactics offered. Refer to your program manager or senior coordinator for the most current schedule.
BUMC-T | |
| Noon Conference | M/F |
| Goldman Rounds | Tu |
| DOM Grand Rounds | W |
| Academic Half Day | Th |
SAVAHCS | |
| Noon Conference | M/F |
| Sim Lab | Tu |
| DOM Grand Rounds | W |
| DOM Grand Rounds | W |
Elective Rotations
- Allergy and Immunology
- Anesthesiology
- Cardiology
- Dermatology
- Endocrinology
- Gastroenterology
- Hematology and Oncology
- Infectious Diseases
- Integrative Medicine
- Nephrology
- Neurology
- Palliative Care
- Pulmonology
- Rheumatology
- Sports Medicine
- Women’s Health
It also is possible to set up a variety of away electives and global electives.
How big is the program?
In a typical year, the program has between 115-125 residents.
Why two hospitals?
We rotate through private, government and public hospitals, giving each resident the opportunity to experience four different practices. Around half of all graduates from university-based residency programs will eventually end up in private practice. We want to make sure each resident has a diversified training experience that will prepare them no matter where they end up practicing.
The university setting provides a highly academic venue to see a very diverse patient population, particularly with very acute pathologies, requiring state-of-the-art interventions and therapeutics. The Tucson VA Medical Center (SAVAHCS) offers residents a chance to see and care for our nation’s veterans on a beautiful campus. Arizona has a sizeable community of retirees, particularly in the winter, and many receive their care from the VA. This means excellent access to cardiovascular medicine and exposure to a number of pulmonary and endocrine disorders.
Where do graduates go after graduation?
Graduates pursue a wide range of fellowships, from cardiology (the most-matched fellowship) to rheumatology and all fellowships in-between. Additionally, a number of graduates go on to practice as outpatient providers or hospitalists, depending on their preference.
What is the patient composition?
Patients are all different ages, ethnicities and cultural backgrounds. Residents may see a college sophomore in their continuity clinic, followed by an 80-year-old former astronaut — as Tucson also is home to Davis-Monthan Air Force Base. With regard to race, 45-50% Hispanic, 35-40% non-Hispanic white, 10% Native American, 2-5% Asian, 2-5% African American.
Our Resident Well-being Incentive is focused on non-medical aspects of resident life in hopes of promoting wellness and work-life balance. This project encourages annual physician visits, healthy eating habits, and exercise and fitness, and promotes camaraderie and team rapport. The overall mission is to promote and maintain a nurturing environment throughout residency by furthering rapport, providing information and access to counseling services to prevent and address burnout, and encouraging residents to be mindful of the importance of their individual well-being.
The program, which draws on wellness principles developed through the Andrew Weil Center for Integrative Medicine and dovetails into many similar aspects at Banner Health’s Cultivating Health in Medicine (CHIM) program, offers tasks on a monthly basis. Previous events have included residency yoga night, dog park gatherings for pet therapy, sound therapy and potluck dinners hosted by current residents. Residents receive conference attendance credit as further incentive for completing resident well-being assignments. During one of the weekly Academic Half Days, a resident well-being lecture is provided to help residents identify fatigue and know the signs of burnout. Residents are also introduced to the housestaff counselor to support mental health. At our institution, we aim to graduate physicians who excel personally as well as professionally.
For more information, reach out to one of your chief residents or Indu Partha, MD, one of the IM Residency Program’s associate directors.
Graduate Medical Education

Learn more about the residency and fellowship programs at the College of Medicine – Tucson.
Training in Tucson
Mary Gosciminski
Program Manager
marygski@arizona.edu
520-626-2761