Department of Medicine
Pulmonary, Allergy, Critical Care and Sleep Medicine
Fellowship Programs
Our fellowship programs offer a balanced clinical and research experience. Our clinical training is enhanced by exposure to a diverse population and subspecialty clinical programs, along with a spectrum of basic science and clinical research opportunities.
The mission of the Allergy and Immunology Fellowship Training Program at the University of Arizona College of Medicine – Tucson is to provide comprehensive, state-of-the-art clinical, research and educational training in allergy and immunology to prepare physicians for successful careers in clinical or academic practice. We accomplish this through the creation of a scholarly environment that promotes research in basic and clinical science, relevant to the medical care of our patients in southern Arizona and the educational needs of our trainees, and by serving as consultants and educators for our peers and students.
Our ACGME-accredited Allergy and Immunology Fellowship program is divided into clinical (50%), research (25%) and educational (25%) activities over 24 months of training. We strive to train outstanding clinicians, successful academicians and noted educators.
Our curriculum includes outpatient and inpatient clinical rotations for pediatric and adult patients at the Banner – University Medical Center Tucson campus and Banner’s Wilmot Pediatric Subspecialty clinics. Elective rotations are available in many subspecialty areas. Our curriculum emphasizes active fellow engagement in both hypothesis-driven research projects and quality-improvement activities.
Didactic/interactive learning activities are framed by the ACGME Allergy-Immunology Program Requirements and Core Competencies, and are foregrounded by topic recommendations from the American Board of Allergy. Our clinical and basic science faculty members support clinical rotations, teach core curriculum topics and provide research mentorship. Fellows may attend local, state and national meetings of our medical societies, including the Arizona Allergy Society, ACAAI and AAAAI.
Each fellow is required to develop and complete a hypothesis-driven research project under the supervision of faculty mentor(s), with the goal to submit a manuscript for peer-reviewed publication.
Each fellow will also be required to write one scholarly work such as a review, book chapter or case report/series, under faculty mentorship, with at least one scholarly work submitted for presentation at a national conference.
Quality-improvement, patient safety and disparities-reduction activities are emphasized. Each fellow will be required to develop a structured, faculty-mentored project wherein they identify an area within the context of allergy-immunology practice, education or research for intervention, design and implement an improvement plan, and report the outcome.
- Banner – University Medical Center Tucson, 1625 N. Campbell Ave., Tucson, AZ 85719
- Diamond Children’s Banner University Medical Center Tucson, 1625 N. Campbell Ave., Tucson, AZ 85719
- Banner – University Medicine North, 3838 N. Campbell Ave., Building 2, Tucson, AZ 85719
PGY-5
PGY-4
| Sean Timothy Tully, DO | 2025 | DO: Marian University College of Osteopathic Medicine, Indianapolis, 2019 |
| Yasamin N. Ghiasi, MD | 2024 | MD: Albany Medical College, New York, 2019 Residency: Scripps Clinic/Scripps Green Hospital, San Diego, Internal Medicine, 2022 |
| Jelena Eremija, MD | 2023 | MD: University of Belgrade College of Medicine, Serbia, 2010 Residency: University of Arizona College of Medicine – Tucson, Pediatrics, 2021 |
| Alexander Nicholson, MD | 2022 | MD: Oregon Health and Science University School of Medicine, 2017 Residency: University of Hawaii, Internal Medicine, 2020 |
| Sanjay Patel, DO | 2021 | DO: University of Pikeville-Kentucky College of Osteopathic Medicine, 2015 Residency: University of Louisville, Kentucky, Internal Medicine, 2018 |
| Nora Odisho, DO | 2020 | DO: University of North Texas Health Science Center at Fort Worth/Texas College of Osteopathic Medicine Residency: Banner – University Medical Center Phoenix/Phoenix Children’s Hospital, Internal Medicine/Pediatrics |
Program Director
Core Faculty
Candidates must be a graduate of a certified Accreditation Council for Graduate Medical Education (ACGME) residency program in internal medicine, pediatrics or a combined internal medicine-pediatrics program, and must be board certified or board eligible for that program.
Fellowship applications will be accepted through the Electronic Residency Application Service (ERAS) online service that transmits applications and supporting documentation for U.S. fellowship matching positions. Selections are announced as part of the NRMP Fellowship Match in December. You must apply through ERAS and register for participation in the match through the NRMP Fellowship Medical Specialties Matching Program.
- Program number is 0200300001
- Number of fellows per year: 2
- Length of fellowship: 2 years
- Opportunities available for third year, research track
Application Requirements
- ERAS application
- Personal statement
- Three current letters of recommendation from people you’ve worked with in the last year
- Must have passed USMLE (Steps 1, 2 and 3) or COMLEX to be considered for an interview
- The PGY-level is set for the program, not the individual. All fellows in PCCM and CCM programs enter as a PGY-4 regardless of their previous experience.
International Medical Graduates
Highly qualified international medical graduates are welcome to apply to the program. In addition to the above requirements, they must have a standard ECFMG Certificate from the Educational Commission for Foreign Medical Graduates.
Fellows must have either U.S. citizenship or permanent residency status. This fellowship program is unable to accept candidates with H1B or J-1 visas.
Timeline and Deadlines
All applicants are reviewed through ERAS, internal and external candidates alike. The program reviews all applications and selects the most qualified candidates for an interview.
- June: Programs open for fellowship applicants (see the MyERAS® Fellowship User Guide)
- Mid-July: ERAS PostOffice opens to July cycle programs
- August: Interviews begin
- December: Match results available for July application cycle programs
What to Expect
It is generally recommended that applicants start gathering application materials in January to be ready to apply by July. ERAS begins transmitting applications to the fellowship programs in early to mid-July. It is highly recommended that your application be completed and submitted by this point. The application review process starts the last week of July through August. Interview offers go out shortly after the review process. Interviews occur over a 6-8 week period beginning the last week of August through October. This time frame may vary depending on the application deadlines for ERAS and NRMP. Rank lists are due in mid-November and the match announcement is in early December.
A fellow accepts appointment as a clinical assistant in the program. It is understood that appointments at the University of Arizona College of Medicine – Tucson are year-to-year, and subject to annual renewal, pursuant to Chapter 4, University Handbook for Appointed Personnel and the Arizona Board of Regents Policy Manual, 6-301, et seq.
All accepted candidates will undergo an onboarding process through Banner – University Medicine and the University of Arizona College of Medicine – Tucson Graduate Medical Education Office.
Preferred Criteria
Our program emphasizes the three pillars of the University of Arizona – Banner University Medical Group mission: patient care, research and education. Strong candidates for this program will show a history of excellence in at least one of these areas:
- Clinical expertise
- Quality improvement
- Clinical, translational or basic science research
- Education leadership
The ACGME-accredited three-year Pulmonary and Critical Care Medicine program consists of a diverse clinical experience that meets the directives of the American Board of Internal Medicine requirements and prepares our fellows for subspecialty board examination and certification.
Inpatient Experience
Inpatient hospital services are divided among three campuses: Banner – University Medical Center (UMC) Tucson, Banner – UMC South and the Southern Arizona VA Health Care System (SAVAHCS). Each venue offers critical care services in a closed ICU model (MICU) and pulmonary consult services. The critical care service is an admitting service for patients with a broad array of critical illnesses. The pulmonary consult service provides expertise in the management of acute and chronic pulmonary conditions for other admitting services upon request.
The MICU team is composed of an attending physician, pulmonary fellow, residents and medical students. The pulmonary consult service is generally composed of an attending and fellow and may have a resident or medical student, and provides consultative services to all programs and services within Banner – UMC and outside affiliates, while SAVAHCS provides consultative services within the VA system.
In addition to these core services, fellows also rotate through a procedures service and a thoracic surgery and lung transplant service (MICU C), and will have the opportunity to rotate through a variety of electives. On the procedures service, fellows will work with an interventional pulmonologist and gain firsthand experience in cutting-edge procedures including airway management, rigid bronchoscopy, stent placement, argon plasma coagulation (APC), bronchial thermoplasty, pleuroscopy, pleural drainage catheter placement, endobronchial ultrasound (EBUS), navigational bronchoscopy and percutaneous tracheostomy. The MICU C service is composed of a transplant or interventional pulmonology attending, a PA and occasionally a fellow. Fellows participate in the primary management of lung transplant patients, including new transplants and post-transplant complications, as well as the care of patients admitted for thoracic surgery. Elective opportunities are ample and enable fellows to develop and expand skills relevant to the practice of pulmonary and critical care medicine.
Outpatient Experience
Pulmonary clinics are located at the Banner locations and SAVAHCS. Fellows follow their own template of ambulatory patients in the pulmonary clinic under the supervision of an attending physician. All fellows attend clinic longitudinally throughout their three years of training. Interesting or difficult patients are reviewed during the weekly clinical conference. In addition to their continuity clinic, second- and third-year fellows rotate through our sub-subspecialty clinics to gain further clinical exposure to these patients. These clinics include pulmonary hypertension, lung transplantation, lung cancer, cystic fibrosis, interstitial lung disease, sleep medicine, allergy and immunology, and palliative care. Additional outpatient experiences include pulmonary function test interpretation, cardiopulmonary exercise testing and pulmonary rehabilitation services.
During the initial period of clinical experience, fellows familiarize themselves with various research opportunities. Fellows pursue a research project during the second and third years of their training. This project can be in either clinical or bench research. Selection of a project is guided by consultation with the fellowship director and other members of the division.
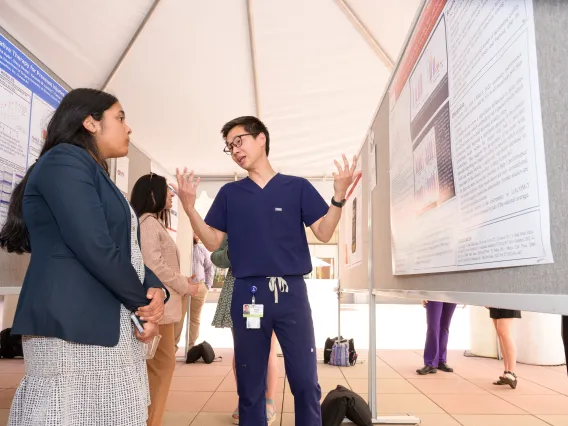
The research progress of the fellow during the second and third years of fellowship is monitored and facilitated through biannual presentations before a Scholarship Committee.
- Banner – University Medical Center Tucson, 1625 N. Campbell Ave., Tucson, AZ 85719
- Banner – University Medical Center South, 2800 E. Ajo Way, Tucson, AZ 85713
- University of Arizona Cancer Center – North Campus, 3838 N. Campbell Ave., Tucson, AZ 85719
- Southern Arizona VA Health Care System, 3601 S. 6th Ave., Tucson, AZ 85723
PGY-6
PGY-5
PGY-4
| Name | Grad Year | Education |
|---|---|---|
| Seyed “Sohail” Habibi Pasdar, MD | 2025 | MD: Azad University, Teheran, Iran, 2008 |
| Andre Johnson, MD, PhD | 2025 | MD: Texas A&M University Naresh K. Vashisht College of Medicine, Bryan, Texas, 2019 Residency: University of California, Riverside, Internal Medicine, 2022 |
| Marni Sarazen, MD | 2025 | MD: Medical College of Wisconsin, Milwaukee, 2019 Residency: University of Arizona College of Medicine – Tucson, Internal Medicine, 2022-2025 |
| Waseem Albasha, MD (chief fellow) | 2024 | MD: University of Arizona College of Medicine – Tucson, 2016 Residency: University of Arizona College of Medicine – Phoenix, Internal Medicine, 2019 Fellowship: University of Arizona College of Medicine – Tucson, Nephrology, 2021 |
| Sooraj Kumar, MBBS | 2024 | MBBS: S.R.M. Medical College Hospital and Research Centre, India, 2016 Residency: University of Arizona College of Medicine South Campus, Internal Medicine, 2021 |
| Bhargav Patel, MD | 2024 | MD: Paul L. Foster School of Medicine, Texas Tech University, 2018 Residency: University of Arizona College of Medicine – Tucson, Internal Medicine, 2021 |
| John A. Sandoval, MD | 2024 | MD: Universidad Autonoma de Guadalajara, Mexico 2006 Residency: University of Arizona College of Medicine South Campus, Internal Medicine, 2016 |
| Sarah M. Upson, MD, MBA (chief fellow) | 2024 | MD: St. George’s University School of Medicine Grenada Residency: NY Presbyterian Brooklyn Methodist Hospital/Weil Cornell Medical College, Internal Medicine, 2021 |
| Nicholas Klimberg, MD | 2023 | MD: New York Medical College, 2016 Residency: University of California Davis Health System, Internal Medicine, 2019 |
| Jyotirmayee Lenka, MD | 2023 | MBBS: Maharaja Krishna Chandra Gajapati Medical College, India Residency: Rochester General Hospital, New York, Internal Medicine |
| John Rathbun, MD | 2023 | MD: University of New Mexico School of Medicine, 2017 Residency: University of New Mexico School of Medicine |
| Ashley Marie Scott, MD | 2023 | MD: Michigan State University College of Human Medicine, 2017 Residency: Henry Ford Hospital/Wayne State University |
| Allison Wright, DO | 2023 | DO: Arizona College of Osteopathic Medicine of Midwestern University, 2017 Residency: University of New Mexico School of Medicine |
| Arista Chand, MD | 2022 | MBBS: University of Sydney Medical School, 2014 Residency: Greenwich Hospital Greenwich, Connecticut, 2019 |
| Benjamin Gerke, MD | 2022 | MD: Loma Linda University School of Medicine, California, 2016 Residency: Mayo Clinic College of Medicine and Science, Rochester, Minnesota, 2019 |
| Angela Gibbs, MD | 2022 | MD: University of Washington School of Medicine, 2015 Residency: Providence St. Vincent Portland, Internal Medicine, 2018 |
| Benjamin J. Jarrett, MD, MPH | 2022 | MD: Ross University School of Medicine, Portsmouth, Dominica, 2014 Residency: University of Arizona College of Medicine – Tucson, 2018 |
| Kelly Wickstrom, DO | 2021 | DO: Des Moines University-Osteopathic Medical Center, 2015 Residency: University of Arizona College of Medicine – Tucson, Internal Medicine, 2018 |
| Bryan Austin Borg, MD | 2020 | MD: University of Arizona College of Medicine – Tucson, 2014 Residency: University of Colorado School of Medicine, Internal Medicine, 2017 |
| Jonathan K. Callaway, MD | 2020 | MD: University of Arizona College of Medicine – Tucson, 2014 Residency: Mayo Clinic Phoenix, Internal Medicine, 2017 |
| Faraz Jaffer, MD | 2020 | MD: Ross University School of Medicine, Dominica, 2014 Residency: University of Arizona College of Medicine – Tucson, South Campus, Internal Medicine, 2017 |
| David C. Miller, MD | 2020 | MD: University of Pittsburgh School of Medicine, 2014 Residency: Beth Israel Deaconess Medical Center, Harvard Medical School, Internal Medicine, 2017 |
| Sasan Sazgar, MD, MBA | 2020 | MD: Shahid Beheshti University of Medical Sciences, Iran, 2008 Residency: Rochester Regional Health, Unity Health System, Internal Medicine, 2013 |
Our Pulmonary and Critical Care Fellowship Program participates in the Electronic Residency Application Service (ERAS). Our ACGME Program ID is 156-03-21-001. Interviews are currently virtual/remote. You must apply through ERAS and register for participation in the match through the NRMP Fellowship Medical Specialties Matching Program.
Selections will be announced as part of the NRMP Fellowship Match in December. All accepted candidates must obtain an Arizona postgraduate training permit (see Licensure) from the Arizona Medical Board.
Application Requirements
- ERAS or NRMP application
- Personal statement
- Three current letters of recommendation from people you’ve worked with in the last year
- Must have passed USMLE (Steps 1, 2 and 3) or COMLEX to be considered for an interview
- The PGY-level is set for the program, not the individual. All fellows in PCCM and CCM programs enter as a PGY-4 regardless of their previous experience.
International Medical Graduates
International medical graduates are welcome to apply to the program. In addition to the above requirements, they must have a standard ECFMG Certificate from the Educational Commission for Foreign Medical Graduates.
Fellows must have either U.S. citizenship, permanent residency status or a valid J-1 visa status. This fellowship program is unable to accept candidates with H1B visas.
Timeline and Deadlines
All applicants are reviewed through ERAS, internal and external candidates alike. The program reviews all applications and selects the most qualified candidates for an interview.
- June: Programs open for fellowship applicants (see the MyERAS® Fellowship User Guide)
- Mid-July: ERAS PostOffice opens to July cycle programs
- August: Interviews begin
- December: Match results available for July application cycle programs
What to Expect
It is generally recommended that applicants start gathering application materials in January to be ready to apply by July. It is highly recommended you have taken “Step III” (pre-boards residency exam). ERAS begins transmitting applications to the fellowship programs in early to mid-July. It is highly recommended that your application be completed and submitted by this point. The application review process starts the last week of July through August. Interview offers go out shortly after the review process. Interviews occur over a 6-8 week period beginning the last week of August through October. This time frame may vary depending on the application deadlines for ERAS and NRMP. Rank lists are due in mid-November and the match announcement is in early December.
A fellow accepts appointment as a clinical assistant in the program. It is understood that appointments at the University of Arizona College of Medicine – Tucson are year-to-year, and subject to annual renewal, pursuant to Chapter 4, University Handbook for Appointed Personnel and the Arizona Board of Regents Policy Manual, 6-301, et seq.
All accepted candidates will undergo an onboarding process through Banner – University Medicine and the University of Arizona College of Medicine – Tucson Graduate Medical Education Office.
The Critical Care Medicine (CCM) fellowship is a two-year ACGME-accredited track within the Pulmonary and Critical Care Fellowship program. The program ID for CCM Track in NRMP/ERAS: 1015156F1
We offer critical care training to qualified internists, medical subspecialists and emergency medicine physicians. The fellow will develop and refine the multiple skills necessary for the successful management of complex and critically ill patients in the medical, trauma/surgical and cardiovascular intensive care units (ICUs). In addition, the fellow will gain familiarity and competence in the management of post-operative cardiothoracic and other surgical patients.
The fellow will become proficient in advanced airway management, ultrasound use in critical care medicine, bronchoscopy and fiber optic airway techniques, advanced ventilator and alternative gas exchange modes, and extracorporeal membrane oxygenation (ECMO), and will have elective time to pursue individual interests within critical care as well as develop research interests of their own.
Highlights of our fellowship program include a recent American Thoracic Society Innovations in Fellowship Education award for our Comprehensive Airway Management Training Program. In addition, our ECMO program is recognized as an Extracorporeal Life Support Organization Center of Excellence with a robust regional presence and referral base.
Fellows will be prepared to take the ABIM/ABEM Critical Care Medicine board examination.
Educational Activities
Educational activities include a weekly pulmonary/CCM case presentation and didactic session, a quarterly combined CCM conference with colleagues in surgical/trauma CCM, a monthly journal club and a monthly Morbidity and Mortality ICU conference. In addition, a series of topical lectures and hands-on simulation and training will be provided for airway management and critical care ultrasound experiences.
Clinical Experience
Clinical fellowship activities include rotations at Banner – University Medical Center (UMC) Tucson and Banner – UMC South.
The clinical activities and responsibilities of the critical care medicine fellows focus on the development of an evaluation and management plan for critically ill patients and the supervision and teaching of residents in the intensive care unit. CCM fellows are required to see and participate in the initial assessment and management of all patients admitted to, or evaluated in consultation by, the ICU service. Progressive independence during the fellowship provides senior fellows increasing opportunity to direct patient care and teaching. Fellows will gain proficiency in the evaluation and management of critically ill and injured patients with medical, surgical, traumatic and neurological diseases.
Evaluation and management of acute and chronic respiratory failure involves differential diagnoses, ventilator management and diagnostic approaches. This includes evaluation and management of patients with:
- Acute respiratory distress syndrome
- Acute and chronic respiratory failure in obstructive lung diseases
- Neuromuscular respiratory drive disorders
- Acute lung injury due to trauma
- Invasive and non-invasive modes of ventilation
- Circulatory and shock disorders including septic, cardiogenic and hypovolemic shock
- Cardiovascular diseases including ischemic heart disease, sepsis and sepsis syndromes, hypertensive emergencies
- Multi-organ failure
- Acute metabolic disturbances and electrolyte and acid-base disorders
- Inhalation or radiation induced lung injury
- Infections in the immunosuppressed patient
- Anaphylaxis and acute allergic reactions
- Respiratory failure including ARDS, acute and chronic respiratory failure in patients with obstructive and restrictive lung diseases, and in those with neuromuscular respiratory drive disorders
- Use of paralytic drugs and sedative and analgesic medications
- Hemodynamic and ventilatory support of patients in the post-operative period
- Overdoses and intoxication syndromes
- Metabolic, nutritional and endocrine effects of critical illness
- Hematologic and coagulation disorders associated with critical illness
- Detection and prevention of iatrogenic and nosocomial problems in critical care medicine
- Psychosocial and emotional effects of critical illness on patients and families
- Management of end-of-life issues and palliative care
- Evaluation and management of patients with neurosurgical and trauma emergencies
- Critical obstetric and gynecologic disorders
- Trauma
- Neurosurgical emergencies
- Obstetric and gynecologic disorders
- Evaluation and management of patients after discharge from the ICU
- Evaluation and management of patients with disorders of the cardiovascular, respiratory, renal, gastrointestinal, genitourinary, neurologic, endocrine, hematologic, musculoskeletal and immune systems
- Evaluation and management of infectious diseases in the ICU
- Basic and advanced cardiopulmonary resuscitation (CPR)
- Procedures: Fellows have the opportunity to perform and supervise a variety of critical care procedures including arterial lines, central venous lines, pulmonary artery catheterization, endotracheal intubation, bronchoscopy, chest tube placement, thoracentesis, paracentesis, lumbar puncture and percutaneous tracheostomy
Elective clinical rotations for fellows include: Difficult Airway Management, Advanced Echocardiography, Thoracic Surgery and Lung Transplantation, Pulmonary Hypertension (including performing right heart catheterization), Medical Toxicology, Palliative Medicine and a variety of medical subspecialties.
Research Experience
Each fellow is expected to participate in quality-improvement activities related to the care of critically ill patients.
Varied faculty interests afford the fellow broad exposure to a variety of investigative opportunities. Current clinical areas of interest include quality-improvement projects regarding sepsis, ICU delirium, airway management, and safety and critical care ultrasound in shock.
Fellows are required to develop and complete a hypothesis-driven research project under the supervision of faculty mentor(s), with the goal of submission of a manuscript for peer-reviewed publication.
Each fellow will also be required to write one scholarly work such as reviews, book chapters and case report/series, under faculty mentorship, with at least one scholarly work submitted for presentation at a national conference.
Quality-improvement, patient safety and disparities-reduction activities are emphasized.
Each fellow will be required to develop a structured, faculty-mentored project to identify an area within the context of critical care medicine practice, education or research that requires intervention, and to devise and implement a plan for improvement.
Completion of Training
The fellow will be able to independently perform care in the ICU and also be adequately versed in the indications, contraindications, techniques, strengths and limitations of each procedure and the management of any complications. Fellows will learn the tenets of stabilization of critically ill patients and understand the differential diagnoses and appropriate diagnostic evaluations of such patients. They will both lead and function within interdisciplinary teams to provide care that is timely, appropriate and takes into account patient or family preferences. The humanistic and caring concern for each patient, family and medical issue is an essential component of taking care of patients in the ICU.
Not including health care partner organizations, affiliated community practices and providers, and mobile clinic services, our physicians practice and teach at two major facilities:
- Banner – University Medical Center Tucson, 1625 N. Campbell Ave., Tucson, AZ 85719
- Banner – University Medical Center South, 2800 E. Ajo Way, Tucson, AZ 85714
PGY-5
PGY-4
| Name | Grad Year | Education |
|---|---|---|
| Stephen Joseph Crabbe, MD | 2025 | MD: University of Arizona College of Medicine – Tucson, 2020 Residency: Advocate Health Care/Advocate Christ Medical Center Program, Emergency Medicine, 2023 |
| Jad Dandashi, MD, MPH | 2024 | MD: Texas A&M University System Health Science Center College of Medicine, 2018 Residency: Henry Ford Hospital, Emergency Medicine, 2021 |
| Paul Crawford, MD | 2023 | MD: The Ohio State University College of Medicine, 2018 Residency: Banner University of Arizona, Emergency Medicine, 2020 |
| Terence Potter, DO | 2023 | DO: Lake Erie College of Osteopathic Medicine, Ohio, 2018 Residency: Maricopa Medical Center, Phoenix, Emergency Medicine, 2021 |
| Zachary Hernandez, MD | 2021 | MD: Stanford School of Medicine, 2015 Residency: University of Arizona College of Medicine – Tucson, Emergency Medicine, 2018 |
| Rebecca Milligan, MD | 2019 | MD: University of New Mexico School of Medicine, 2014 Residency: University of Arizona College of Medicine – Tucson, Emergency Medicine, 2017 |
| Katelin Morrissette, MD | 2018 | MD: Medical College of Wisconsin, 2013 Residency: Dartmouth Hitchcock Medical Center, Emergency Medicine, 2016 |
| Jeremy Greenberg, MD | 2017 | MD: University of Arizona College of Medicine – Tucson, 2012 Residency: Vanderbilt University Medical Center, Emergency Medicine, 2014 |
| Raj R. Joshi, MD | 2016 | MD: Ross University School of Medicine, 2011 Residency: University of Arizona College of Medicine – Tucson, Emergency Medicine |
| Cameron D. Hypes, MD, MPH | 2015 | MD: Ohio State University, 2010 Residency: Henry Ford Hospital, Chief Resident, Emergency Medicine, 2013 |
| Sage Whitmore, MD | 2014 | MD: Baylor College of Medicine, 2009 Residency: Vanderbilt University Medical Center, 2012 |
| Eric Chase, MD | 2013 | MD: Wayne State University School of Medicine, 2008 Residency: University of Arizona College of Medicine – Tucson, Emergency Medicine, 2011 |
| Jarrod M. Mosier, MD | 2012 | MD: University of Nevada School of Medicine, 2007 Residency: University of Arizona College of Medicine – Tucson, Emergency Medicine, 2010 |
Fellowship applications will be accepted through the Electronic Residency Application Service (ERAS) online service that transmits applications and supporting documentation for U.S. fellowship matching positions. All interviews and selection of candidates will be coordinated through ERAS and matched through NRMP. The CCM program appears in ERAS along with the PCCM.
- Program number is 1560321001
- Number of fellows per year: 1
- Length of fellowship: 2 years
- Opportunities available for third year, research track
Application Requirements
- Graduate from a certified ACGME-accredited residency program
- Current curriculum vitae
- Letter of interest in training in critical care medicine
- Recent photograph
- Copy of USMLE or COMLEX scores
- Copy of ECFMG Certificate (if applicable; see International Medical Graduates below)
- Copy of medical school transcript and diploma
- Three letters of recommendation (one from program director and at least one from an internist)
- The PGY-level is set for the program, not the individual. All fellows in PCCM and CCM programs enter as a PGY-4 regardless of their previous experience.
International Medical Graduates
International medical graduates are welcome to apply to the program. In addition to the above requirements, they must have a standard ECFMG Certificate from the Educational Commission for Foreign Medical Graduates.
Fellows must have either U.S. citizenship, permanent residency status or a valid J-1 visa status. This fellowship program is unable to accept candidates with H1B visas.
What to Expect
The program reviews all applications and selects the most qualified candidates for an interview. Fellowship interviews generally begin in August. Appointments are announced in December.
A fellow accepts appointment as a clinical assistant in the program. It is understood that appointments at the University of Arizona College of Medicine – Tucson are year-to-year and subject to annual renewal, pursuant to Chapter 4, University Handbook for Appointed Personnel and the Arizona Board of Regents Policy Manual, 6-301, et seq.
All accepted candidates must obtain an Arizona postgraduate training permit (see Licensure) from the Arizona Medical Board.
Preferred Criteria
Emergency medicine residents applying from ACGME-accredited emergency medicine programs should have completed at least six months of direct patient care experience in internal medicine, of which at least three months must have been in a medical ICU. This is an ACGME requirement.
Fellows entering at the F1 (first-year fellow) level who have completed an ACGME-accredited emergency medicine program, but have not completed the prerequisite clinical experiences in internal medicine, must complete these experiences during the beginning of the F1 year.
Our one-year ACGME-accredited Sleep Medicine Fellowship Program is committed to excellence in sleep medicine training. Fellows become proficient sleep physicians and learn to deliver excellent patient-centered care, interpret sleep studies and manage an interdisciplinary team.
The fellow will learn to diagnose and treat patients with a wide range of sleep and circadian rhythm disorders. The program ensures that findings from recent studies, including health services and patient-centered outcomes research, is translated into practice. It provides training for fellows who come from different disciplines in all aspects of sleep medicine. Trained sleep medicine faculty are board-certified in sleep medicine with backgrounds in pulmonary, pediatrics, psychiatry, psychology and neurology.
Our faculty are committed to advancing knowledge in sleep medicine by conducting the highest quality basic, clinical and translational research. Thus, the program consists of a diverse clinical experience that meets ABIM requirements and prepares our fellows for successful subspecialty board examination and certification.
The fellow will have clinical rotations at different sleep clinics during the 12-month fellowship period. There are two sites with opportunity to do elective rotations. Banner – University Medical Center Tucson’s Center for Sleep Disorders includes very busy sleep clinics and a four-bed sleep laboratory that performs laboratory- and home-based sleep studies. The Southern Arizona Veterans Affairs Health Care System (SAVAHCS) is a 15-minute drive to South Tucson and also includes a four-bed sleep laboratory.
Under the supervision of a faculty member, the fellow will evaluate and manage patients with sleep disorders, with an emphasis on continuity of care and care coordination that is patient-centered with that underscores excellence in management of patients with sleep disorders. The fellow will interpret polysomnography with the supervising faculty member during the weekdays.
The fellow will maintain a log of all interpretations of polysomnographic studies and Multiple Sleep Latency Test/Maintenance of Wakefulness Tests (MSLTs/MWTs) and other diagnostic tests that include home sleep studies and positive airway pressure therapy downloads — all of which they will interpret under supervision. Additionally, they will receive one-on-one teaching during their supervised sleep clinics (half-day once a week). At the start of the fellowship, they will receive twice-a-week lectures for the first three months for a total of 24 lectures (“summer intensive lecture series”). Over the rest of the year, they will attend lectures and case presentations during the monthly and highly interdisciplinary sleep conference, which has representation from psychology, pediatric pulmonary, nursing, psychiatry, neurology, ENT surgery, trauma surgery and nutritional sciences. They will have access to sleep atlases, audio-visual learning tools and online seminars for self-reading.
Research Activity
Sleep medicine fellows are encouraged to participate in scholarly activities, including clinical, translational and basic science research that would lead to peer-reviewed publications and research presentations at national and international meetings.
Additionally, the fellow has an opportunity to participate in community outreach and education as well as bedside education of rotating resident physicians, medical and undergraduate students. Participation in various forms of patient-oriented research is possible with a gamut of ongoing interdisciplinary research activities that are ongoing in the division, Banner – University Medical Center’s Center for Sleep Disorders and the University of Arizona Health Sciences Center for Sleep & Circadian Sciences. Additionally, participation in quality-improvement activity, journal club and hands-on training in scientific writing is feasible.
The program leadership will be happy to assist fellows in finding a mentor to guide them through such scholarly activity. Progress of scholarly activities will be reviewed at monthly fellowship meetings as well as during the biannual meetings with the fellowship program director.
The major Sleep Medicine Fellowship training sites are Banner – University Medical Center Tucson and South clinical facilities, Banner – University Medicine North, Building 2, and the Southern Arizona VA Health Care System (SAVAHCS), with its flagship Tucson VA Medical Center.
The research facility most associated with our program is the Center for Sleep, Circadian & Neuroscience Research. Its studies include the immunology of sleep, sleep in the critically ill, and the psychological aspects of sleep and disorders that affect it, including obstructive sleep apnea and insomnia.
| Name | Grad Year | Education |
|---|---|---|
| Tingrui Wang, MD | 2025 | MD: Peking Union Medical University, China, 2013 Residency: St. Joseph’s Hospital & Medical Center, Phoenix, 2015-2018 |
| Muhammad Ebrahim Khan, MBBS | 2024 | MBBS: Army Medical College, Rawalpindi, Pakistan, 2007 Residency: Guthrie Robert Packer Hospital, Sayre, Pennsylvania, Internal Medicine, 2015 |
| Michael William, MD | 2023 | MD: American University of Antigua College of Medicine Residency: Northwell Health Zucker School of Medicine, Internal Medicine |
| Taaha Rafi, MD | 2022 | MD: Windsor University School of Medicine, 2018 Residency: Southern Illinois University School of Medicine, 2021 |
| Kirstin Alexis Robertson, MD | 2021 | MD: Medical College of Wisconsin, Milwaukee, 2016 Residency: University of Arizona College of Medicine – Phoenix, Internal Medicine/Pediatrics, 2020 |
| Lauren E. Estep, MD | 2020 | MD: Pennsylvania State University College of Medicine, Hershey, 2013 Residency: University of Illinois, Chicago, Internal Medicine, 2016 |
Candidates interested in the Sleep Medicine Fellowship Program must apply through the Electronic Residency Application Service (ERAS). Selections are announced as part of the NRMP Fellowship Match in December. You must apply through ERAS and register for participation in the match through the NRMP Fellowship Specialties Matching Service.
Qualifications for admission include:
- The successful completion of a three-year ACGME-accredited residency
- U.S. citizenship, valid residency or J-1 visa (this fellowship program is unable to accept candidates with H1B visas)
- Graduates of foreign medical schools must have a standard ECFMG Certificate
- All accepted candidates must obtain an Arizona postgraduate training permit (see Licensure) from the Arizona Medical Board
For your information:
- Our program number: 5200314002
- Number of fellows per year: 1
- Length of fellowship: 1 year
- Opportunities available for an extra year, research track
- All fellows in sleep medicine enter as a PGY-4 regardless of their previous experience
Application Requirements
- Personal statement
- Three letters of reference (LOR)
- CV
- USMLE or COMLEX scores
- ECFMG certificate (see “International Medical Graduates,” below)
- Medical school transcript
- Certificate of completion (or good standing in) ACGME-accredited residency
International Medical Graduates
International medical graduates are welcome to apply to the program. In addition to the above requirements, they must have a standard ECFMG Certificate from the Educational Commission for Foreign Medical Graduates.
Fellows must either have U.S. citizenship, valid U.S. residency or a J-1 visa. This fellowship program is unable to accept candidates with H1B visas.
Timeline and Deadlines
The ERAS and National Residency Matching Program (NRMP) websites have information for fellowship application and match registration deadlines. It is generally recommended applicants begin gathering their application materials in January in order to be ready to apply by July. It is highly recommended you have taken “Step III” (pre-boards residency exam). ERAS begins transmitting applications to the fellowship programs in early to mid-July. It is highly recommended that your application be completed and submitted by this point. The application review process starts the last week of July through the month of August. Interview offers go out shortly after the review process. Interviews occur over a 6-8 week period starting the last week of August through the last week of October. This time frame may vary depending on the application deadlines for ERAS and NRMP. Rank lists are due in mid-November and the match announcement is in early December.
A fellow accepts appointment as a clinical assistant in the program. It is understood that appointments at the University of Arizona College of Medicine – Tucson are year-to-year, and subject to annual renewal, pursuant to Chapter 4, University Handbook for Appointed Personnel and the Arizona Board of Regents Policy Manual, 6-301, et seq.
This basic-translational research fellowship track is for outstanding trainee candidates in adult and pediatric pulmonary medicine. It offers an extra year in any of our four fellowships and is focused on an intensive research project culminating in a grant submission. Research experience is desired but not a prerequisite.
Training the next generation of physician-scientists is our highest priority. For those fellows interested in cutting-edge research, our division, the Asthma & Airway Disease Research Center and the BIO5 Institute have partnered to offer a dedicated four-year research fellowship for highly qualified individuals. This position is made available on an every-other-year cycle and is often unfilled due to the rigorous selection process and the nature of the research training experience.
The Asthma & Airway Disease Research Center is internationally known for pioneering work defining the genetic origins of asthma since its founding in 1971. Asthma & Airway Disease Research Center projects span all spheres of research: clinical trials through their NIH-funded Asthma Clinical Research Center (ACRC), translational research using our unique cohort and technology-driven bench research. Our recent success engineering humanized mice will revolutionize the way we study human disease.
If selected, trainees entering the third year are expected to apply for career development awards and will be in an excellent position to become thought leaders in pulmonary research both on campus and on the national stage.
Applicants to any of the four fellowships available in the Division of Pulmonary, Allergy, Critical Care and Sleep Medicine and participating in the Electronic Residency Application Service (ERAS) may be selected as a candidate for this track based upon their research interests and qualifications.
Training in Tucson

Learn more about the residency and fellowship programs at the College of Medicine – Tucson.

Applications are listed as the University of Arizona Program for the July application cycle.
Helen Hill
Fellowship Programs Manager
520-626-6114
mhhill@arizona.edu



![[Kaitlyn Elizabeth Leahey, DO]](/sites/default/files/styles/az_medium/public/2025-08/Leahey_Kaitlyn-DO_25_0840.jpg.webp?itok=qDsX616g)
![[Tara F. Carr, MD]](/sites/default/files/styles/az_medium/public/2025-06/CARR-TARA-MD_PACCS-1516_NHG-06242024_5x7.jpg.webp?itok=McuVh92i)



![[Shannon Brewer, DO]](/sites/default/files/styles/az_medium/public/2025-08/Brewer_Shannon_PACCS-7-Edit_26_0837.jpg.webp?itok=i_FwN0ZR)
![[Adam Knox, MD]](/sites/default/files/styles/az_medium/public/2025-08/Knox_Adam_PACCS-7-Edit_26_0837.jpg.webp?itok=Dkf61xlY)
![[Alexander J. Somers, DO]](/sites/default/files/styles/az_medium/public/2025-08/Somers_Alexander_PACCS-7-Edit_26_0837.jpg.webp?itok=lh-I2ZcG)




![[Oluwafunmilola (Funmi) T. Alabi, MBChB]](/sites/default/files/styles/az_medium/public/2025-08/Alabi_Oluwafunmilola_PACCS-7-Edit_25_0856.jpg.webp?itok=HKTTRo3w)