Neurology
Fellowship Programs
We offer a one-year, ACGME-accredited fellowship in clinical epilepsy through the Arizona Comprehensive Epilepsy Program (ACEP). This program provides advanced training in the evaluation and management of patients with epilepsy across both inpatient and outpatient settings.
Fellows gain in-depth experience in medical and surgical aspects of epilepsy care, including patient selection and assessment for epilepsy surgery. They develop proficiency in interpreting a full range of EEG modalities — standard, ambulatory, video-EEG monitoring and ICU monitoring — as well as in advanced neurophysiological techniques such as electrocorticography, evoked potentials and functional cortical mapping.
The fellowship includes exposure to neuroimaging, neurostimulation and Wada testing with quantitative EEG analysis. Fellows also have the option to rotate through the pediatric neurology clinic and the neurological ICU for additional specialized training.
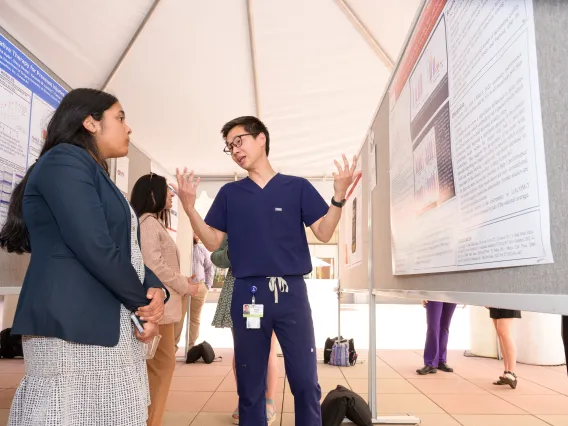
In addition to clinical work, the program emphasizes scholarly activity. Fellows are encouraged to participate in clinical trials and engage in basic research in cellular neurophysiology and molecular biology, with a focus on developing novel therapeutic strategies.
As a participating physician in ACEP, the fellow becomes an integral part of a multidisciplinary team dedicated to delivering comprehensive epilepsy care and advancing the field through education and research.
Why Us?
- Comprehensive Clinical Training: As part of the Arizona Comprehensive Epilepsy Program (ACEP), our fellowship offers broad exposure to all aspects of epilepsy care — from initial diagnosis to advanced surgical interventions. Fellows work with a diverse patient population across inpatient, outpatient, ICU and pediatric settings, gaining hands-on experience in complex and challenging cases.
- Cutting-Edge Technology and Techniques: Our program provides advanced training in neurophysiological diagnostics, including video-EEG monitoring, quantitative EEG, functional mapping and neuroimaging. Fellows also gain exposure to innovative treatments such as neurostimulation and investigational drug trials.
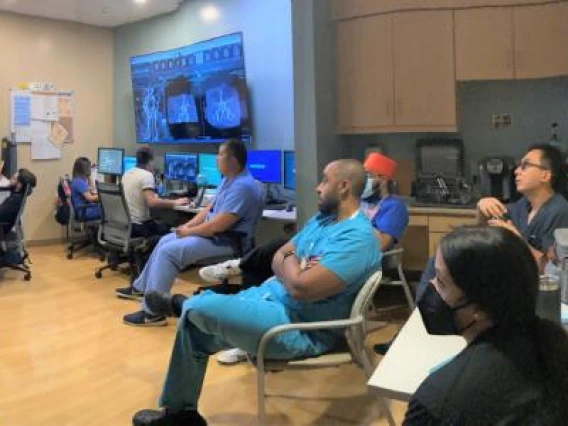
- Collaborative, Multidisciplinary Environment: Fellows are integral members of a multidisciplinary team that includes epileptologists, neurosurgeons, neuroradiologists, neuropsychologists and researchers. This collaborative environment ensures a well-rounded and supportive training experience.
- Research Opportunities and Academic Growth: We encourage scholarly activity and offer robust opportunities in both clinical and basic science research. Fellows can contribute to ongoing clinical trials or engage in laboratory research focused on cellular neurophysiology and molecular biology, helping to advance the future of epilepsy treatment.
- Mentorship and Career Development: Our faculty is committed to mentoring fellows in both clinical excellence and academic development. Whether your goal is academic medicine, private practice or research, we provide personalized guidance to help shape your future career.
- ACGME-Accredited Excellence: As an ACGME-accredited program, we adhere to the highest standards of education and training. Graduates leave fully prepared to pursue board certification in epilepsy and assume leadership roles in the field.
The epilepsy fellow will be scheduled for 12 one‐month rotations to include the following:
| Epilepsy Clinic | 9 Blocks |
| Inpatient Epilepsy | 1 Block |
| Children’s Clinic | 1 Block |
| Elective | 1 Block |
Examples of elective rotations include research, sleep medicine, neuropsychiatry and epilepsy surgery. Throughout all rotations, the fellow will be responsible for reading outpatient and inpatient EEGs
under the supervision of the epilepsy faculty.
Fellows learn to treat patients with medically intractable epilepsy, including:
- Long-term subdural/video EEG monitoring to localize the epileptic focus in the brain
- Subdural/video-EEG grid monitoring and cortical mapping procedures
- Resective surgery
- Corpus callosotomy
- Vagus nerve stimulation
- Minimally invasive MRI-guided laser surgery
Our epileptologists provide comprehensive clinical evaluation and treatment of epilepsy. Patients who are identified as medically refractory are discussed in a multidisciplinary conference including neurology, neurosurgery (epilepsy surgery), neuropsychology and neurophysiology to determine if a referral should proceed for neurosurgical evaluation and treatment.
The primary site for the fellow’s education is the University of Arizona and our affiliated hospital, Banner University Medical Center Tucson (BUMC-T). In addition, fellows’ education also takes place at Banner University Medical Center South and North Campus (BUMC-SC/NC), Children’s Clinics for Rehabiliative Services, and Southern Arizona VA Health Care Center (SAVAHCS).
How to Apply
To be eligible for this fellowship, candidates must have completed an ACGME-accredited neurology residency.
Physicians interested in our Fellowship Programs at the University of Arizona may apply through the Electronic Residency Application Service (ERAS). You may find additional information on how to apply to fellowships through ERAS.
Your ERAS application will require the following documentation:
- Up-to-date CV
- Three letters of reference
- USMLE/COMLEX 1, 2 and 3 scores
- ECFMG certificate
- Medical school transcript
- MSPE (Dean’s letter)
- Certificate of completion (or good standing in) ACGME-accredited residency
- Personal statement
For international applicants: We only sponsor J-1 visa applicants.
During this one-year ACGME-accredited program, fellows acquire advanced knowledge in clinical neurophysiology, specifically EMG/NCS and EEG. As part of their training, fellows obtain clinical skills in evaluating, diagnosing, and treating neuromuscular and epilepsy patients. As part of their education, fellows will learn botulinum toxin injection techniques, neuromuscular ultrasound and continuous EEG. Fellows are required to attend lectures and neurophysiology review sessions and take the AANEM self-assessment examination.
Fellows have the choice of focusing on EMG or EEG, including clinical experience. Even with clinical focus, fellows will develop competency in both fields.
- EMG-predominant fellows will gain expertise in performing EMG/NCS, NMUS and the use of botulinum toxin injections. They receive clinical experience in the management of neuromuscular patients, including ALS, acquired neuropathies and muscular dystrophies. There is the opportunity for research, and each fellow will see patients in a broad variety of clinics and inpatient settings. At the end of their training, fellows are eligible to sit for both the ABEM and ABPN-added qualifications in Clinical Neurophysiology Boards.
- EEG-predominant fellows will learn epilepsy patient management and to expertly read and interpret EEGs. These fellows will learn EM, EEG, continuous EEG and have exposure to sleep medicine. They will see patients from a variety of adult and pediatric clinics and learn outpatient and inpatient seizure management. They will be board eligible in the ABPN-added qualifications in Clinical Neurophysiology Boards.
The one-year fellowship curriculum includes:
- Outpatient EMG
- Outpatient neuromuscular clinics, including ALS multidisciplinary clinic
- Outpatient EEG
- Inpatient EEG and cEEG
- Outpatient epilepsy clinic
Other curriculum elements: Sleep medicine, botulinum toxin injection for spasticity, NM ultrasound
- Banner – University Medical Center North, 3838 N. Campbell Ave., Building 2, Tucson, AZ 85719
- Banner – University Medical Center South, 2800 E. Ajo Way, Tucson, AZ 85713
To be appointed to a fellow in a clinical neurophysiology position, the candidate must successfully complete medical school training, pass USMLE Steps I, II and III, and graduate from ACGME-accredited neurology or pediatric neurology residency program. Foreign medical graduates are also required to complete the ECFMG certification. The program director verifies with the applicant’s current institution that they are a resident in good standing. Three letters of recommendation are required and reviewed. The GME office must approve each accepted fellow. Each fellow’s academic credentials are verified before being accepted into the program.
Physicians interested in the Clinical Neurophysiology Fellowship Program may apply through the American Accrediation of Neuromuscular & Electrodiagnostic Medicine.
We offer a one-year, ACGME-accredited fellowship in vascular neurology through the Banner – University Medical Center Tucson, the only Joint Commission certified comprehensive stroke center in southern Arizona. This program provides advanced training in the diagnosis, treatment and prevention of cerebrovascular diseases across both inpatient and outpatient settings.
Fellows gain extensive hands-on experience managing the full spectrum of stroke care, including hyperacute treatment, secondary prevention, rehabilitation planning and outpatient follow-up. They develop expertise in acute stroke therapies such as intravenous thrombolysis, mechanical thrombectomy and neurocritical care management of complex cerebrovascular cases.
Training includes direct involvement in stroke codes, multidisciplinary stroke rounds, and exposure to advanced neuroimaging techniques, including CT/MRI perfusion and vessel imaging. Fellows also participate in specialized clinics focused on post-discharge stroke care, young stroke and stroke in cancer patients.
The fellowship offers optional rotations in neuroradiology, neurocritical care, inpatient stroke and research, allowing fellows to tailor their experience to their career goals. The program also incorporates structured education in quality improvement, stroke systems of care and health disparities in stroke treatment.
In addition to clinical responsibilities, the fellowship emphasizes academic scholarship. Fellows are encouraged to participate in institutional research initiatives, including retrospective studies, stroke registry analyses and investigator-initiated projects, with opportunities for publication and national conference presentations.
As part of the Comprehensive Stroke Center team, fellows become integral members of a multidisciplinary group dedicated to providing evidence-based, patient-centered care and advancing the field of vascular neurology through education, innovation and research.
Why Us?
Comprehensive Clinical Training: As part of a comprehensive stroke center, our fellowship offers exposure to a wide range of stroke presentations — from transient ischemic attacks to large vessel occlusions and complex secondary prevention cases. Fellows are fully involved in emergency stroke management, inpatient care, outpatient follow-up and the ongoing development of our telestroke services.
Advanced Diagnostics and Acute Therapies: Fellows train in state-of-the-art diagnostic tools, including CT/MRI angiography, perfusion imaging and the ongoing development of our transcranial Doppler program. They gain deep experience in hyperacute stroke interventions such as thrombolysis, thrombectomy decision-making and critical care management.
Collaborative, Multidisciplinary Environment: Fellows work within a highly collaborative team of neurologists, neurosurgeons, emergency medicine physicians, neuroradiologists, neuropsychologists and neurointensivists. This interdisciplinary approach enhances clinical decision-making and fosters a supportive learning environment.
Research and Scholarly Activity: We offer robust opportunities for scholarly engagement. Fellows may participate in clinical trials or lead studies focused on cryptogenic stroke, atrial disease, stroke disparities or systems-based outcomes. Mentorship is provided by faculty with national expertise in stroke research.
Mentorship and Career Development: Our faculty are committed to guiding fellows in achieving their professional goals, whether in academic medicine, clinical leadership or research. Fellows benefit from personalized mentorship, involvement in quality initiatives, teaching opportunities and leadership development.
ACGME-Accredited Excellence: As an ACGME-accredited program, we uphold the highest standards of training in vascular neurology. Graduates are well-prepared to pursue board certification and to take on leadership roles in stroke care delivery and innovation.
Fellows will learn to treat:
- Ischemic stroke
- Transient ischemic attacks
- Intracerebral hemorrhage
- Carotid stenosis
- Aneurysms and subarachnoid hemorrhage
- Vascular malformations of the brain and spinal cord
Fellows will participate in an array of services, including:
- administration of intravenous tPA (clot-busting medicine) and mechanical clot retrieval for acute ischemic stroke
- neurosurgical and vascular procedures
- medication management for stroke prevention
- rehabilitation services
The vascular neurology fellow will be scheduled for 12 one-month rotations to include the following:
| Stroke Wards | 6 Blocks |
| Neurosurgery Wards | 1 Block |
| Neurocritical Care Wards | 1 Block |
| Neurorehabilitation | 1 Block |
| Interventional and Diagnostic Neuroradiology | 1 Block |
| Elective | 2 Blocks |
Tools and Technology
- multimodal CT scanning
- magnetic resonance imaging (MRI)
- magnetic resonance angiography
- digital angiography
- carotid duplex and transcranial doppler ultrasound
The primary site for the fellows’ education is the University of Arizona and our affiliated hospital, Banner – University Medical Center Tucson (BUMCT), the only Joint Commission certified Comprehensive Stroke Center in southern Arizona. BUMCT is also the only trauma center and the only tertiary, academic referral center in the greater Tucson region. Stroke clinics are held at the North Campus outpatient facility and the neurorehabilitation rotation is held at Encompass Health Rehabilitation Institute of Tucson.
Program Director
Program Faculty
Program Coordinator
Positions and Duration
The Vascular Neurology Fellowship is a 12-month program beginning on July 1 and ending on June 30. Two positions are offered on a competitive basis each year.
Eligibility Criteria
Candidates are selected for the fellowship program based on specific prerequisites and criteria:
- Graduation from an ACGME-accredited residency program, American Osteopathic Association (AOA)-approved residency program, ACGME International (ACGME-I) Advanced Specialty Accreditation program, Royal College of Physicians and Surgeons of Canada (RCPSC)-accredited or College of Family Physicians of Canada (CFPC)-accredited residency program located in Canada.
- Fellows must have successfully completed a program in neurology, child neurology or neurodevelopment disabilities that satisfies the requirements above.
- Additionally, candidates must be either a U.S. citizen, possess an employment authorization document (EAD), or be eligible for a J-1 visa.
Fellow Selection
How to Apply
Your ERAS application will require the following documentation:
- Up-to-date CV
- Three letters of reference
- USMLE/COMLEX 1, 2 and 3 scores
- ECFMG certificate
- Medical school transcript
- MSPE (Dean’s letter)
- Certificate of completion (or good standing in) ACGME-accredited residency
- Personal statement
Fellows will be appointed only when academic credentials have been verified.
International Medical Graduates
Timeline and Deadlines
The program participates in the National Resident Matching Program and adheres to its policies and principles. Applications must be submitted through the Electronic Residency Application Service. Application submissions begin December 1. The program will review and applications and extend interviews through March. Match Day for vascular neurology fellowships occurs in mid-May, with training beginning the following academic year on July 1.
Training in Tucson
Learn more about the residency and fellowship programs at the College of Medicine – Tucson.

Applications are listed as the University of Arizona Program for the July application cycle.
Regina Goeller
Program Manager, Residency
RGoeller@neurology.arizona.edu